Case Report Published on December 30, 2022
Mucocele Beyond Frontal Sinus: A Case Report
Vivek Sasindran, Migha K P
1. Department of ENT, Head and Neck Surgery, Pushpagiri Institute of Medical Sciences & Research Centre, Thiruvalla;
2. PG Resident, Pushpagiri Institute of Medical Sciences & Research Centre, Thiruvalla*
ABSTRACT
Unilateral maxillary sinusitis with a dental origin is a commonly seen condition both in the otorhinolaryngology and dental outpatient settings. Failure to recognize Odontogenic Maxillary Sinusitis (OMS) can cause intractable sinusitis leading to grave complications.1
INDRODUCTION
A mucocele is an epithelium-lined mucus-filled sac, characterized by expansion of the sinus cavity and remodeling of the sinus walls. They are cystic structures, lined by pseudostratified or ciliated columnar epithelium.1 benign paranasal sinus lesion rarely extending intracranially.2 Obstruction of the outflow tract of the involved sinus with an inflammatory process occur within the sinus leading to the formation of mucoceles.3 Mucoceles may invade nearby structures if there is associated bone erosion. Most commonly mucoceles occur in the frontal sinus (60-65%)4 because drainage pathway is complex and narrow. Etiology is multifactorial, most common cause is sinus surgery (66-86%).5 Diagnosis is based on clinical examination and imaging modalities (CT/MRI). Endoscopic marsupialization is the advisable surgical choice. The following case is a large frontal mucocele with intracranial and intraorbital extension with anterior frontal sinus table defect.
CASE REPORT
27-year-old female presented with c/o swelling over forehead right side with bulging of right eyeball for 1 year associated with occasional pain, double vision and persisting headache on frontal region. The swelling was of Insidious onset and gradually progressive in size. No history of nasal symptoms, loss of vision, watering from eyes. No history of previous nasal surgeries, trauma to the head or face. On local examination, A Swelling approximately 8x6 cm visualized on right frontal region extending in to the right orbit with proptosis (Figure 1), pushing eyeball downwards with upper eyelid oedema and congested conjunctiva. On palpation there was no tenderness or local rise of temperature. The swelling was firm in consistency, transilluminant and fluctuant in nature. Eyeball movement was restricted on superior, medial, and lateral direction. Nasal endoscopy revealed high septal deviation with bilateral inferior turbinate hypertrophy.

Figure 1. Front and lateral view of the swelling measuring approximately 8x6 cm size
CT paranasal sinus showed soft tissue density lesion filling and expanding the right frontal sinus with thinning and resorption of frontal bone and intracranial, intraorbital, contralateral frontal sinus extension (Figure 2).

Figure 2. CT paranasal sinuses: Coronal, axial and sagittal view: soft tissue density lesion filling and expanding the right frontal sinus with thinning and resorption of right frontal bone and intra orbital, intracranial and contralateral frontal sinus extension
Patient underwent Endoscopic marsupialization (Figure 3&4). Anterior and posterior ethmoidectomy was done on both sides. Draf IIb approach done and widened the frontal sinus drainage. The contents of mucocele evacuated. Large defect visualized on anterior wall of frontal sinus on right side (Figure 5). Proceeded with Bicoronal approach and anterior frontal wall reconstruction done with titanium mesh (Figure 6). Post operatively, swelling regressed and the patient was symptom free (Figure 7). The patient is still 7 under regular follow up with no further symptoms.
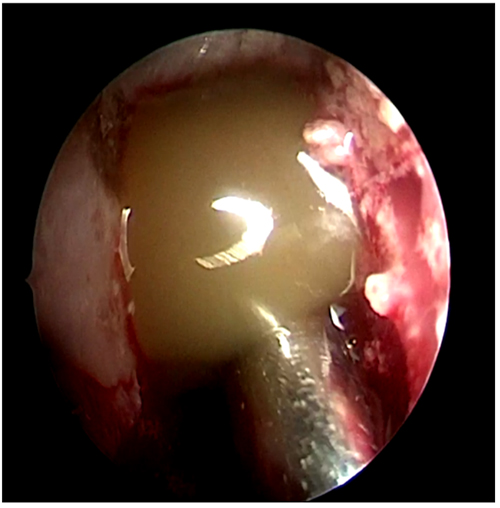
Figure 3. Endoscopic view of frontal mucocele with contents
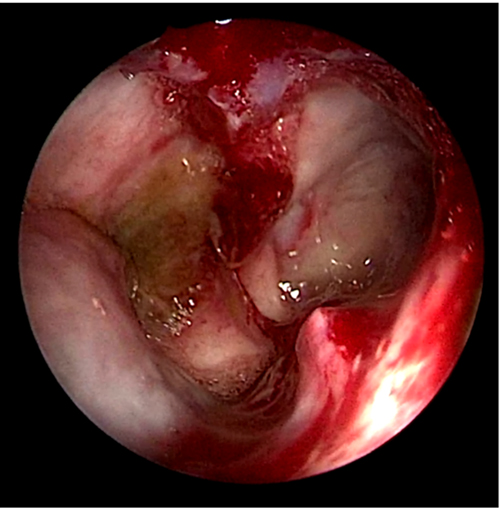
Figure 4. Endoscopic view of right frontal sinus after evacuating the mucocele
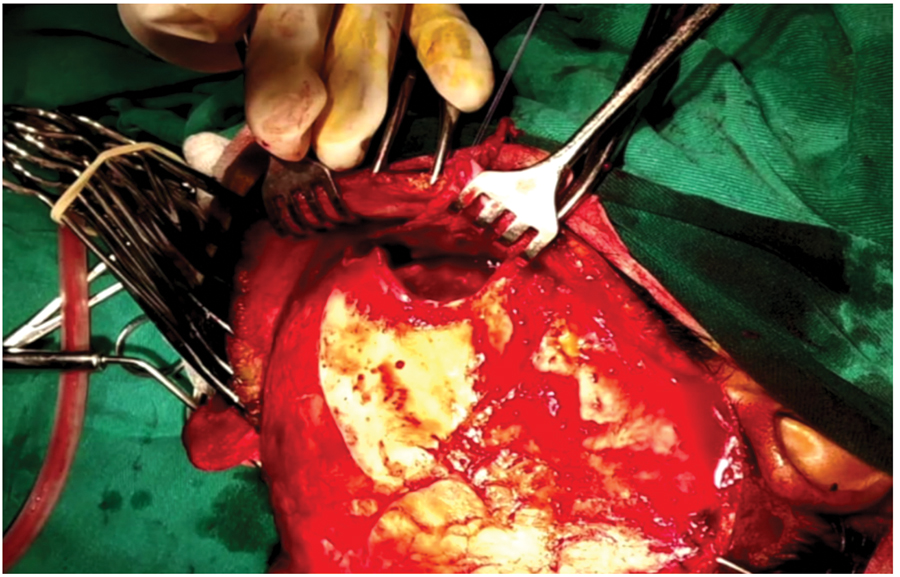
Figure 5. Bicoronal approach, elevating pericranial flap showing large defect in the anterior wall of frontal bone
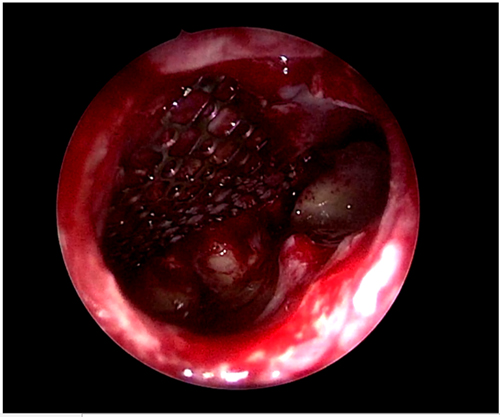
Figure 6. Endoscopic view of anterior wall reconstruction with
titanium mesh

Figure 7. 6-month Postoperative period: Front and lateral view -Resolved frontal swelling
DISCUSSION
Mucoceles are slowly expansile lesion within one of the paranasal sinuses.1 Incidence of mucoceles varying depending upon etiology. In third century, BC Cannalis first described the condition. According to Jaswal et al. mucoceles were first described by Lagenbeck in the 19th century,6 these lesions were first called mucoceles by Rollet in 1896.7 mucoceles can extend into cranial fossa through the skull base or into the orbit through the lamina papyracea. Sex distribution is almost in cases of mucoceles. usually occur in young adults. Mucoceles predominantly affect the frontal sinus (60-65%), followed in order of frequency by the ethmoidal (20-30%), maxillary (10%) and sphenoidal sinuses (2-3%),4 according to a study conducted in France 10–14% cases are due to trauma and 15–17% occur as spontaneously. Majority of mucoceles patients had history of sinus surgery (78%) like Lynch-Howarth, Caldwell-Luc operations 1.5% cases underwent endonasal surgery.3 Concha bullosa, Superior turbinate, Lacrimal sac are the uncommon locations of mucoceles.1
Variable etiology of mucoceles including Idiopathic, previous surgery, chronic sinusitis, allergy and chronic inflammation, head injury and secondary to benign and malignant tumors. Obstructed sinus outflow tract leads to inflammatory process within the sinus. Cytokine IL-1 and TNF are released within the epithelial lining of mucocele. Cytokine leads to osteolytic action and bony erosion8
Clinical features are depending upon involvement of sinuses and extension of disease. Ophthalmological symptoms are usually common than other symptom, periorbital swelling, pain and exophthalmosis are the most common ophthalmological complaints. Limited ocular motility, double vison and visual disturbance are seen in severe displacement of orbital contents. Neurological and nasal symptoms are rare.9 Optic neuropathy reported in 18% patients with intraorbital extension.10 Nasal obstruction, epiphora are other symptoms. Majority cases had past history of sinus surgery or trauma.
Clinical examination and imaging (CT/MRI) are the diagnostic tools of mucoceles. Homogenous, isodense, soft tissue lesions within the involved sinuses and with expansion and bony changes like remodeling, erosions are revealed in CT scan.9 Bony erosion of surrounding structures and extension of disease can be made out with the help of imaging. If suspecting intracranial extension or Sino nasal malignancies MRI can be useful. Mucoceles can be differentiated from surrounding soft tissues with variability of signal intensity in MRI. Low signal intensity lesion is visualized in T1 imaging and high signal intensity in T2 imaging due to high water content of mucocele.11 Imaging that determines the most appropriate surgical approach.
Endoscopic marsupialization is the safest, minimally invasive and first line management of most of the mucoceles.it provide evacuation of mucoceles contents, sinus drainage and ventilation. Large extensive mucoceles may require open techniques or combined approach. The purpose of surgical management of mucoceles are complete evacuation, widening of sinus drainage pathway to avoid recurrence and further complications.
In this case mucocele which extended into intracranial and infraorbital regions, hence open bicoronal approach with endoscopic marsupialization and anterior wall defect reconstruction was done.
CONCLUSION
The Mucoceles can remain asymptomatic for a long period of time. The disease is benign and treatable but the early diagnosis is of extreme importance. CT/MRI are the imaging methods that determine the selection of appropriate surgical approach. Endoscopic surgery is a safe treatment method with excellent result. Large extensive mucoceles may require combined approach.
End Note
Author Information
- Dr. Vivek Sasindran (MBBS, MS ENT) Professor Department of ENT, Head and Neck Surgery
Pushpagiri Institute of Medical Sciences & Research Centre, Thiruvalla. - Dr. Migha K P (MBBS) PG Resident
Pushpagiri Institute of Medical Sciences & Research Centre, Thiruvalla.
Conflict of Interest: None declared
Acknowledgement: The authors declared there is no existing conflict of interest in this case report.
References
1. Arrué P, Kany MT, Serrano E, Lacroix F, Percodani J, Yardeni E, et al. Mucoceles of the paranasal sinuses: uncommon location. The Journal of Laryngology & Otology. 1998 Sep;112(9):840–4.
[Crossref]
2. Nakayama T, Mori K, Maeda M. Giant pyocele in the anterior intracranial fossa--case report. Neurol Med Chir (Tokyo). 1998 Aug;38(8):499–502.
[Pubmed] | [Crossref]
3. Bockmühl U, Kratzsch B, Benda K, Draf W. Surgery for paranasal sinus mucocoeles: efficacy of endonasal micro-endoscopic management and long-term results of 185 patients. Rhinology. 2006 Mar;44(1):62–7.
[Pubmed]
4. Obeso S, Llorente JL, Pablo Rodrigo J, Sánchez R, Mancebo G, Suárez C. [Paranasal sinuses mucoceles. Our experience in 72 patients]. Acta Otorrinolaringol Esp. 2009;60(5):332–9.
[Pubmed] | [Crossref]
5. Khong JJ, Malhotra R, Selva D, Wormald PJ. Efficacy of endoscopic sinus surgery for paranasal sinus mucocele including modified endoscopic Lothrop procedure for frontal sinus mucocele. J Laryngol Otol. 2004 May;118(5):352–6.
[Pubmed] | [Crossref]
6. Waizel-Haiat S, Díaz-Lara IM, Vargas-Aguayo AM, Santiago-Cordova JL. Experience in the surgical treatment of paranasal sinus mucoceles in a university hospital. Cirugía y Cirujanos. 2017 Jan 1;85(1):4–11.
[Crossref]
7. Cansiz H, Yener M, Güvenç MG, Canbaz B. Giant Frontoethmoid Mucocele with Intracranial Extension: Case Report. Ear Nose Throat J. 2003 Jan;82(1):50–2.
[Crossref]
8. Lund VJ, Henderson B, Song Y. Involvement of cytokines and vascular adhesion receptors in the pathology of fronto-ethmoidal mucocoeles. Acta Otolaryngol. 1993 Jul;113(4):540–6.
[Pubmed]
9. Lee TJ, Li SP, Fu CH, Huang CC, Chang PH, Chen YW, et al. Extensive paranasal sinus mucoceles: a 15-year review of 82 cases. Am J Otolaryngol. 2009;30(4):234–8.
[Pubmed] | [Crossref]
10. Kim YS, Kim K, Lee JG, Yoon JH, Kim CH. Paranasal sinus mucoceles with ophthalmologic manifestations: a 17-year review of 96 cases. Am J Rhinol Allergy. 2011;25(4):272–5.
[Pubmed] | [Crossref]
11. Van Tassel P, Lee YY, Jing BS, De Pena CA. Mucoceles of the paranasal sinuses: MR imaging with CT correlation. AJR Am J Roentgenol. 1989 Aug;153(2):407–12.
[Pubmed] | [Crossref]