Case Report Published on December 30, 2022
“THE BROKEN TOOTH” - Case Series on Unilateral Maxillary Sinusitis
Revathy Sajai1, Arjun G Menon1, Sumam P Vazhapilly1, Nevil Varghese1
1. Department of Otorhinolaryngology, Amala Institute of Medical Sciences, Thrissur, Kerala*
ABSTRACT
Unilateral maxillary sinusitis with a dental origin is a commonly seen condition both in the otorhinolaryngology and dental outpatient settings. Failure to recognize Odontogenic Maxillary Sinusitis (OMS) can cause intractable sinusitis leading to grave complications.1
INTRODUCTION
Inflammation of the maxillary antrum due to a viral, bacterial or fungal aetiology is known as maxillary sinusitis. It can be either acute or chronic. But when the cause is a dental or dentoavleolar aetiology with involvemement of floor and cavity of maxillary sinus it is known as OMS. The treatment modality of this form of sinusitis is different from the non odontogenic sinusitis.1
Air filled cavities which develop from the facial bones are known as para nasal sinuses. There are four pairs of sinuses- maxillary, ethmoid, frontal and sphenoid. These sinuses mature with age. Their mucosa contains goblet cells and secrete mucus which facilitate alveolar gas exchange, humidify inspired air, traps particulate matter. The mucociliary action of the respiratory epithelium clears mucus from the sinuses.2
Here we report a case series of 4 patients who presented to us with OMS of odontogenic origin.
Case 1
A 54 year old male presented with complaints of recurrent left sided headache, fever and left purulent nasal discharge since past 4 years. He had a history of trauma to the nose and upper jaw following a road traffic accident 4 years back and the symptoms began soon after the incident. He was being treated with antibiotics during each flare up, with resolution of symptoms. On examination he had tenderness over left maxillary sinus and was febrile. Diagnostic nasal endoscopy showed thick purulent discharge from the left maxillary ostium. CT PNS revealed mucosal thickening in left maxillary sinus along with a hyperdense area (Figure 1). He underwent Left FESS under GA. Thick pus was drained from the left maxillary sinus along with a broken maxillary tooth (Figure 2). Post operatively he was treated with antibiotics. He became symptomatically better during the hospital stay.

Figure 1. CT PNS showing mucosal thickening of left maxillary sinus along with a hyperdense region ( broken tooth)

Figure 2. Endoscopic removal of broken tooth during left middle meatal antrostomy
*Middle turbinate
Case 2
A 14 year old female presented to the ophthalmology department with swelling and pain over the left eye and left side of face associated with blurring of vision and watering of left eye since 1 day. She was referred to ENT for further management. She had history of fever and left nasal block, left mucopurulent nasal discharge 1 week back. 2 weeks back she had a history of tooth extraction following dental infection. On examination she had diffuse oedema and tenderness over the left side of face associated with left epiphora and tenderness over left maxillary, ethmoid and frontal sinus (Figure 3). DNE showed thick mucopurulent discharge from left middle meatus. CT PNS revealed mild periorbital soft tissue thickening with fat stranding on left side along with mucosal thickening in left maxillary, ethmoid and frontal sinuses with obliteration of left OMC and frontal recess (Figure 4). She underwent left FESS under GA and thick pus and tiny bits of broken teeth was drained from the left maxillary sinus. Post operatively she was treated with systemic antibiotics and became symptomatically better.

Figure 3. Left preseptal cellulitis as a complication of left acute odontogenic maxillary sinusitis

Figure 4. CT PNS showing mucosal thickening of left maxillary sinus and haziness of left ethmoidal sinus
Case 3
A 21 year old female presented with complaints of severe left sided frontal headache and fever since 2 weeks associated with left nasal block and post nasal drip, not relieved with antibiotics. She had similar episodes in the past, which used to resolve on taking oral antibiotics. On examination her oro-dental hygiene was very poor and multiple caries teeth were seen with tenderness over left upper premolars. Tenderness was elicited over left maxillary and frontal sinus. Diagnostic nasal endoscopy showed thick mucoid discharge from left middle meatus. CT PNS showed mucosal thickening in left maxillary sinus along with a hyperdense area suspected to be an unerupted maxillary tooth. She was treated with iv antibiotics, analgesics and other symptomatic measures. Later she was advised to extract her unerupted tooth and correct the caries teeth to prevent further recurrences.
Case 4
A 28 year old female presented with complaints of foul smelling right side nasal discharge since 3 weeks associated with right sided facial pain and post nasal drip. She had a history of dental extraction (right upper molar) prior to the development of symptoms. She had past history of allergic rhinitis but it is now under control. Diagnostic nasal endoscopy showed mucopurulent discharge from oedematous right middle meatus. CT PNS showed a soft tissue density lesion completely opacifying right maxillary sinus causing widening of the maxillary ostium and extending into right OMC, right frontal, anterior ethmoidal sinus possibly of fungal aetiology (Figure 5). She underwent Right FESS under GA and thick pus with broken tooth was suctioned out from right maxillary sinus (Figure 6). She became symptomatically better during the hospital stay.
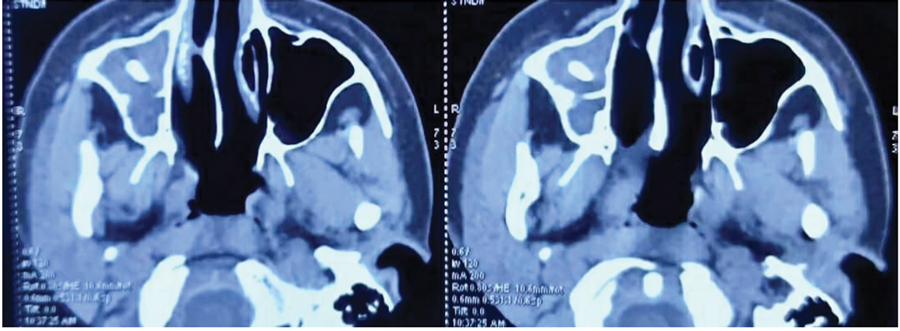
Figure 5. CT PNS showing broken tooth in the right maxillary sinus
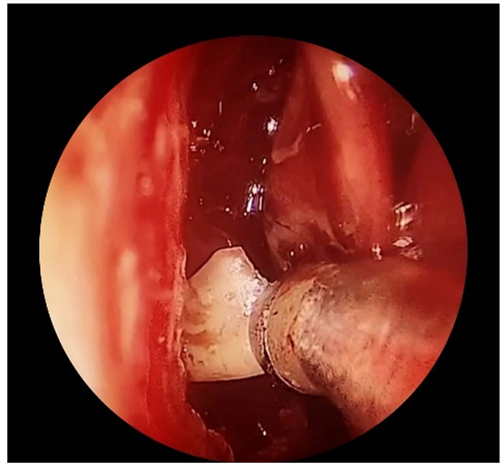
Figure 6. Endoscopic retrieval of broken tooth during FESS
*Middle turbinate
DISCUSSION
Maxillary sinus is the first sinus to develop and is present at birth. It grows from birth to 3 years. Final maturation is attained at 7 to 12 years of age. The ostium of the maxillary sinus opens into the lateral wall of the nasal cavity. Osteomeatal complex (OMC) is a functional unit which forms the final drainage pathway for the anterior group of sinuses. Any disease activity that impairs the function of the OMC can lead to infection and recalcitrant sinusitis in the maxillary sinus and adjacent sinuses.2
Aetiology
In OMS, the microorganisms from the diseased denture destroys maxillary alveolar bone and spread to the maxillary sinus via the lympho-vascular channels leading to inflammation and blockage of the OMC. The main causes are:
1. Iatrogenic
This is the most common cause. Surgeries or procedures involving the dentoalveolar region can compromise the inferior wall of the maxillary sinus leading to an oro-antral communication and can transfer microbes, foreign bodies to the antrum from the oral cavity leading to sinus infection.
2. Endodontic and Periodontic Disease
Pathologies like apical periodontitis, odontogenic cysts, pulpal necrosis and root fracture, periapical cysts, abscesses, or granulomas can cause repeated dental infections and breach the physical barrier of the root of the tooth, spreading to the periapical region, maxillary bone and sinus.3
Clinical features
Major symptoms are unilateral nasal obstruction, foul smelling nasal discharge, bad taste in mouth, post nasal drip, headache, facial pain and occasionally dental pain and hypersensitivity.4
Diagnosis
Appropriate history with supporting physical evidence and radiological imaging can establish the diagnosis. Computed Tomography of the paranasal sinuses can pinpoint the odontogenic origin, foreign body within the maxillary sinus, maxillary sinus floor defect and the diseased tissues.5
Management
The dental aetiology should be managed along with the sinusitis to ensure complete relief and prevent recurrences and complications. Medical and surgical strategies can be adopted together to treat odontogenic sinusitis. To eliminate the source of infection, the root of the tooth must be removed from the sinus or dental infection should be cleared via tooth extraction or root canal therapy. Oral broad spectrum antibiotics is advocated. Functional Endoscopic Sinus surgery is the current gold standard for eradication of the disease. After the sinusitis has been controlled by an otorhinolaryngologist, the dental aetiology has to be dealt with a dentist.5
CONCLUSION
In a patient presenting with unilateral nasal symptoms , the possibility of Odontogenic sinusitis have to be kept in mind. In order to prevent iatrogenic cases, appropriate radiological imaging should be done if a gross anatomic abnormality is suspected.5 In our cases, all the four patients had an odontogenic cause, either broken tooth/teeth or retained teeth which acts as a foreign body and a conduit for microbes. Hence after proper removal of the dental pathology, the patients’ symptoms improved.
End Note
Author Information
- Revathy Sajai, Junior Resident, Department of Otorhinolaryngology, Amala Institute of Medical Sciences, Thrissur, Kerala
- Arjun G Menon, Associate Professor, Department of Otorhinolaryngology, Amala Institute of Medical Sciences, Thrissur, Kerala
- Sumam P Vazhapilly, Assistant Professor, Department of Otorhinolaryngology, Amala Institute of Medical Sciences, Thrissur, Kerala
- Nevil Varghese, Assistant Professor, Department of Otorhinolaryngology, Amala Institute of Medical Sciences, Thrissur, Kerala
Conflict of Interest: None declared
REFERENCES
1. Psillas G, Papaioannou D, Petsali S, Dimas GG, Constantinidis J. Odontogenic maxillary sinusitis: A comprehensive review. J Dent Sci. 2021 Jan;16(1):474–81.
[Pubmed] | [Crossref]
2. Little RE, Long CM, Loehrl TA, Poetker DM. Odontogenic sinusitis: A review of the current literature. Laryngoscope Investig Otolaryngol. 2018 Apr;3(2):110–4.
[Pubmed] | [Crossref]
3. Nandakumar BS, Niles NNA, Kalish LH. Odontogenic Maxillary Sinusitis: The Interface and Collaboration between Rhinologists and Dentists. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2021 Dec;2(4):8.
[Pubmed] | [Crossref]
4. Simuntis R, Kubilius R, Vaitkus S. Odontogenic maxillary sinusitis: a review. Stomatologija. 2014;16(2):39–43.
[Pubmed]
5. Lee KC, Lee SJ. Clinical features and treatments of odontogenic sinusitis. Yonsei Med J. 2010 Nov;51(6):932–7.
[Pubmed] | [Crossref]