Case Report Published on December 30, 2022
Case Series on Covid Associated Mucormycosis
Sarada Sreenath1, Anil Kumar A R2, Saju K G3, Elizabeth T George4
1. Fellowship in Rhinology and Anterior Skullbase Surgery, General Hospital, Ernakulam; 2. Department of ENT, District Hospital, Kannur;
3. Fellowship in Skull Base Surgery (Graz), District Hospital, Thrissur; 4. Department of ENT, General Hospital Ernakulam*
ABSTRACT
Mucormycosis is a rare fungal infection. The rapid increase in the number of cases of mucormycosis during the second wave of covid lead to a new entity called Covid Associated Mucormycosis (CAM). In this case series we discuss 7 cases of CAM who presented to our hospital during the second wave of Covid. We describe their clinical features, investigations, treatment, complications and follow up. Male: Female ratio was 4:3. Mean age of presentation was 57.85. The average time of presentation of symptoms of mucormycosis after covid was 2 weeks. All of them were diabetic. Three of them had cerebral involvement. All of them underwent surgical debridement followed by antifungal therapy. The mortality rate in our study is 42.86 percentage which is compared with other studies in literature. This is the first study of its kind from a government hospital in Kerala
INTRODUCTION
Mucormycosis is an invasive fungal infection. It is caused by fungi of the order Mucorales like Rhizopus, Mucor, Rhizomucor, Cunninghamella and Absidia.1 As the world was struck by Covid 19 infection, there was an abrupt increase in the number of the rare fungal infection mucormycosis being reported. An entity termed Covid Associated Mucormycosis (CAM) came into existence.2 Most of the cases were reported from India. In this case series we describe 7 cases of covid associated mucormycosis including presentation, investigation, management and follow up. This is the first case series on this topic from a government hospital in Kerala (Table 1).

Case 1
A middle-aged female, known diabetic and post COVID presented with nasal block. Nasal endoscopy showed cheesy fungal material in left middle meatus and polypoid nasal mucosa. Specimen from left maxillary sinus showed entangled and broad aseptate fungal hyphae with acute angulation amidst dense inflammatory cells. Necrosis along with necrotic bone fragments were noted (Figure 1). Her MRI brain showed heterogeneously enhancing soft tissue mucosal thickening involving maxillary, frontal, ethmoidal and sphenoid sinuses on left side with intracranial extension of the lesion in basifrontal lobe through cribriform plate. There was small subacute haemorrhage in left frontal lobe (Figure 2). All these findings were suggestive of inflammatory fungal sinusitis consistent with mucormycosis. She underwent endoscopic nasal debridement and was given liposomal amphotericin B followed by oral posaconazole for 1 month. She improved symptomatically and is on follow up. Her nasal endoscopy on follow up was normal and staining from the nasal mucosa did not show any fungal elements.
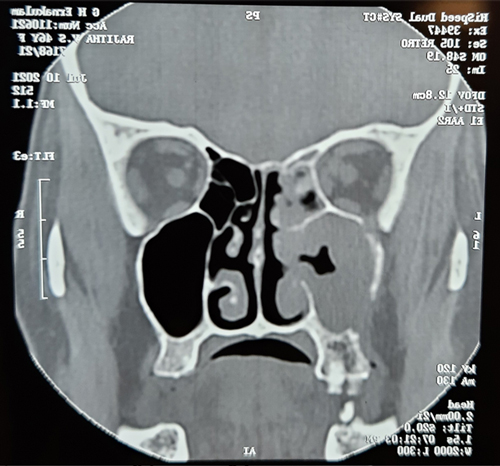
Figure 1. CT scan of case 1. Soft tissue opacification with bony erosion of left maxillary sinus.

Figure 2. MRI of case 1. Heterogenously enhancing mucosal lesion in sinuses with intracranial extension.
Case 2
A 56-year-old lady, known diabetic with history of category B COVID infection presented with complaints of headache and pain around right eye after 20 days of COVID. Diagnostic nasal endoscopy showed purulent nasal discharge in right nasal cavity with oedematous nasal mucosa. Her computed tomography paranasal sinus (CT PNS) showed right maxillary, ethmoid, frontal and sphenoid sinusitis with obliteration of right osteomeatal complex. Magnetic resonance imaging (MRI) brain revealed enhancing irregular mucosal thickening, soft tissue and retained secretions in right maxillary sinus extending to right nasal cavity, ethmoids with subtle erosion of right maxillary sinus with extension to pterygopalatine fossa and orbital apex. She was managed with endoscopic medial maxillectomy and liposomal amphotericin B. Local application of amphotericin was also done. She improved significantly. Her repeat biopsy under nasal endoscopy was normal. She is asymptomatic now at her last follow up.
Case 3
An elderly male patient, known diabetic and hypertensive who had taken intensive care unit (ICU) care for COVID19 infection presented within 2 weeks with complaints of difficulty in opening both eyes, right sided facial pain and right sided loss of vision along with nasal obstruction, nasal discharge and epistaxis. His nasal endoscopy revealed blackish discolouration of both middle turbinates and crusts in bilateral middle meatus. MRI orbit with PNS showed mucosal thickening in bilateral paranasal sinuses, nonenhancing lesions in bilateral middle and left inferior turbinates. On ophthalmologic examination, he had lost perception of light in both eyes and ocular movements were restricted in all directions. Biopsy from the nasal tissue showed necrosis, exudate and abundant mucormycosis with tissue and bone invasion. He underwent complete endoscopic debridement including removal of medial wall of orbit. Patient completed a total dose of 5 g of amphotericin B and then changed to oral posaconazole. But his follow up after 1 month showed crusts in both nasal cavities suggestive of recurrence. Fungal stain from nasal mucosa showed aseptate hyphae which were typical of mucormycosis.
Case 4
A 56-year-old male patient, diabetic and hypertensive turned COVID positive and was under treatment. Two weeks after becoming COVID negative he presented with complaints of nasal congestion and headache. His diagnostic nasal endoscopy revealed black crusts in both nasal cavities (Figure 3). His CT PNS showed mucosal thickening in bilateral maxillary sinuses, bilateral anterior ethmoid air cells, frontal sinus and left sphenoid sinus. Fungal stain from the nasal mucosa showed both aseptate and septate fungal hyphae. Fungal culture and histopathologic examination were suggestive of mixed infection of aspergillus and mucor. Complete surgical debridement of the involved area was done. He was started on liposomal amphotericin B injection along with antibiotics. Frequent endoscopy and local application of antifungals were also done. He developed acute kidney injury after using amphotericin and hence withheld for few days and restarted when his renal parameters became normal. His nasal endoscopy showed complete clearance and he was symptomatically better (Figure 4). But he developed a sudden cardiac arrest and succumbed to death. The most probable cause was acute myocardial infection due to the hypercoagulable state associated with COVID infection.

Figure 3. Preoperative DNE of case 4. Black crust in nasal cavity.
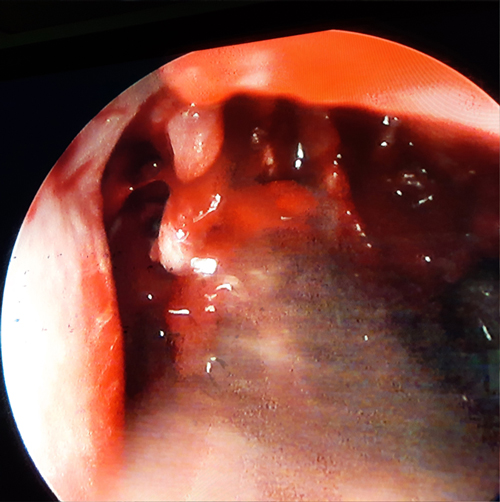
Figure 4. Postoperative DNE of case 4
Case 5
An elderly post COVID lady, diabetic and hypertensive, presented with history of headache, multiple episodes of focal seizures and weakness. CT brain showed acute infarct in left corona radiata and temporal lobe. There was B/L maxillary, ethmoid and sphenoid inflammatory mucosal thickening (Figure 5). MRI brain showed multiple acute infarcts in left temporoparietal region. There was optic nerve hyperintensity on left side. Magnetic resonance angiography (MRA) showed left internal carotid artery (ICA) involvement. Her nasal endoscopy revealed crusts. Fungal staining showed aseptate hyphae. She underwent transnasal decompression and was started on liposomal amphotericin B. She developed a cerebrovascular accident resulting in hemiparesis and later succumbed to death.

Figure 5. MRI of case 5 showing infarct
Case 6
A 57-year-old male patient, known diabetic and hypertensive presented with history of blurred vision and ptosis. At the time of admission to hospital, he was detected as COVID positive. Nasal endoscopy showed crusts in both nasal cavities. CT PNS showed mucosal thickening in right maxillary and ethmoid sinuses with hyperdensities. MRI brain with orbit was consistent with mucormycosis with infiltration of cavernous sinus and orbital apex. His fungal stain and histopathology were consistent with mucormycosis. He was started on liposomal amphotericin B. He underwent complete surgical debridement under nasal endoscopy. But his disease progressed rapidly. He developed cerebrovascular accident. He was in ventilatory support for many days and later succumbed to death.
Case 7
A middle-aged man, known diabetic who suffered COVID pneumonia presented 2 months later with complaints of bilateral eyelid swelling and pain on the right side of the face. His nasal endoscopy showed black crusts in both nasal cavities. He was diagnosed with sinonasal mucormycosis with optic neuritis and underwent endoscopic sinus surgery. Diagnosis was confirmed by calcofluor staining and histopathologic examination of the postoperative specimen from sinuses. He was given liposomal amphotericin B and he showed significant improvement. He is asymptomatic on follow up.
DISCUSSION
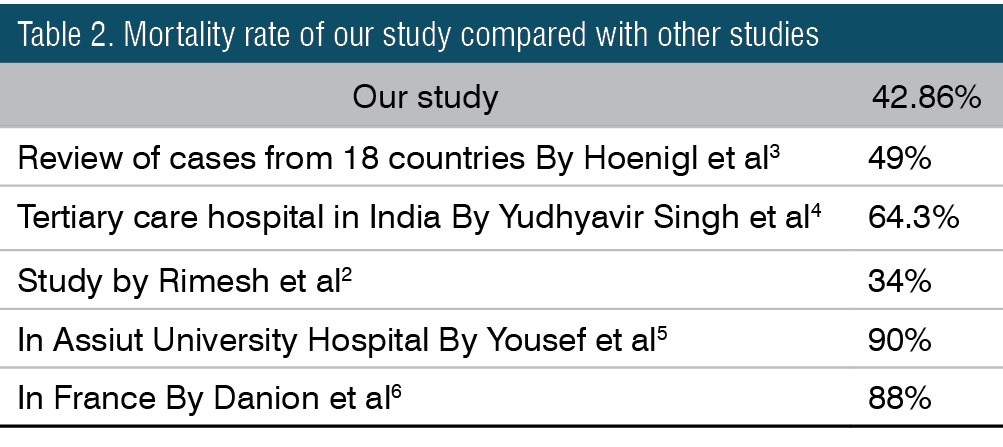
Among the 7 cases of CAM described here, the Male: Female ratio is 4:3. Mean age of presentation is 57.85. Six patients had previous history of covid and one patient was detected covid positive at the time of admission to hospital. The average time of presentation of symptoms of mucormycosis after covid was 2 weeks. All of them were diabetic. All of them were hospitalized for covid treatment. 3 of them had cerebral involvement. All of them underwent surgical debridement followed by antifungal therapy. Mortality in our study is 3 out of 7, ie 42.86% (Table 2). One patient had loss of vision and showed recurrence on last follow up. Rest of the patients are asymptomatic and endoscopy normal.
COVID-19–associated mucormycosis (CAM) has been reported in many countries. CAM constitutes 0.3% of COVID-19 coinfections.7 The case rate of mucormycosis in India; before 2019 was almost 70 times higher than in developed countries. The disease prevalence in India is predicted to be 140 cases per million population.8 Due to the rapid surge of cases during second wave of covid 19, on May 19, 2021, India announced mucormycosis as a notifiable disease under the Epidemic Diseases Act 1897.9 Possible factors contributing to pathogenesis of CAM include impaired phagocytosis, worsened glycemic profile, hyperferritinemic state in covid, rampant use of glucocorticoids and possible dissemination of fungal spores via water used in humidifiers.2
Rhinoorbitocerebral mucormycosis being the most common form of mucormycosis is also the most common reported form of covid associated mucormycosis followed by the pulmonary form.8 The most common CAROCM ( Covid Associated Rhino Orbito Cerebro Mucormycosis) symptoms observed in COSMIC study included orbital/facial pain (23%), oedema (21%), visionloss (19%), ptosis (11%), and nasal congestion (9%). The primary signs included periocular/ facial oedema (33%), vision loss (21%), proptosis (11%), and nasal discharge (10%).10 On histopathology the mucor shows broad (typically 6- to 25- μm diameter), irregular, ribbonlike, non-septate (or sparsely septate) hyphae with irregular broad/right branching. The tissue reaction consist of neutrophil infiltration, vessel invasion and tissue infarction.11
The management of CAM is surgical debridement as adjunct to antifungal therapy.2 The drug of choice to treat mucormycosis is amphotericin B. Posaconazole is the most preferred second line drug.8
End Note
Author Information
- Dr. Sarada Sreenath DLO, DNB, MNAMS
Fellowship in Rhinology and Anterior Skullbase Surgery, Assistant Surgeon,
General Hospital, Ernakulam - Dr. Anil Kumar A.R MS ENT,
Skullbase surgery fellowship (Graz)
Junior Consultant ENT, District Hospital, Kannur - Dr. Saju K.G DLO
Fellowship in Skull Base Surgery (Graz)
Consultant ENT, District Hospital, Thrissur - Dr. Elizabeth T George DLO
Consultant ENT and HOD, General Hospital Ernakulam
Acknowledgement
To all members of Mucor Board GH Ernakulam
Dr. Sujit Harshan, Chief Dental Surgeon, General Hospital, Ernakulam
Dr. Manoj G, Consultant Physician, General Hospital, Ernakulam
Dr. Meena Beevi, Consultant Pathologist, General Hospital, Ernakulam
Dr. Arya R. V, Junior Consultant Microbiology, General Hospital, Ernakulam
Dr. Mini, Consultant Radiologist, General Hospital, Ernakulam
Dr. Rajeendran, Consultant Ophthalmologist, General Hospital, Ernakulam
Dr. Ambili, Consultant Anaesthetist, General Hospital, Ernakulam
Dr. Sandeep V Shenoy, Consultant Nephrologist, General Hospital, Ernakulam
Dr. Dalwin Thomas, Consultant Neurosurgeon, Amrita Hospital, Ernakulam
Dr. Sreeram Prasad. A. V, Consultant Neurologist, Lourdes Hospital, Ernakulam
Conflict of Interest: None declared
Funding: Nil
Ethical Approval: Not required
REFERENCES
1. Revannavar SM, P S S, Samaga L, V K V. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep. 2021 Apr 27;14(4):e241663.
[Pubmed] | [Crossref]
2. Pal R, Singh B, Bhadada SK, Banerjee M, Bhogal RS, Hage N, et al. COVID-19-associated mucormycosis: An updated systematic review of literature. Mycoses. 2021 Dec;64(12):1452–9.
[Pubmed] | [Crossref]
3. Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux JP, et al. The emergence of COVID-19 associated mucormycosis: a review of cases from 18 countries. Lancet Microbe. 2022 Jul;3(7):e543–52.
[Pubmed] | [Crossref]
4. Singh Y, Ganesh V, Kumar S, Patel N, Aggarwala R, Soni KD, et al. Coronavirus Disease-Associated Mucormycosis from a Tertiary Care Hospital in India: A Case Series. Cureus. 2021 Jul;13(7):e16152.
[Pubmed] | [Crossref]
5. Farghly Youssif S, Abdelrady MM, Thabet AA, Abdelhamed MA, Gad MOA, Abu-Elfatth AM, et al. COVID-19 associated mucormycosis in Assiut University Hospitals: a multidisciplinary dilemma. Sci Rep. 2022 Jun 21;12:10494.
[Pubmed] | [Crossref]
6. Danion F, Letscher-Bru V, Guitard J, Sitbon K, Dellière S, Angoulvant A, et al. Coronavirus Disease 2019-Associated Mucormycosis in France: A Rare but Deadly Complication. Open Forum Infect Dis. 2022 Feb;9(2):ofab566.
[Pubmed] | [Crossref]
7. Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS One. 2021;16(5):e0251170.
[Pubmed] | [Crossref]
8. Aranjani JM, Manuel A, Abdul Razack HI, Mathew ST. COVID-19-associated mucormycosis: Evidence-based critical review of an emerging infection burden during the pandemic’s second wave in India. PLoS Negl Trop Dis. 2021 Nov;15(11):e0009921.
[Pubmed] | [Crossref]
9. Palanisamy PR, Elango D. COVID19 associated mucormycosis: A review. J Family Med Prim Care. 2022 Feb;11(2):418–23.
[Pubmed] | [Crossref]
10. Sen M, Honavar SG, Bansal R, Sengupta S, Rao R, Kim U, et al. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India - Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1. Indian J Ophthalmol. 2021 Jul;69(7):1670–92.
[Pubmed] | [Crossref]
11. Meher R, Wadhwa V, Kumar V, Shisha Phanbuh D, Sharma R, Singh I, et al. COVID associated mucormycosis: A preliminary study from a dedicated COVID Hospital in Delhi. Am J Otolaryngol. 2022;43(1):103220.
[Pubmed] | [Crossref]