Case Report Published on December 28, 2024
Labyrinthine Ossificans and Cochlear Implantation in a Case of Post Modified Radical Mastoidectomy
Muhammad Noushad1, Vinay Thampuran P1, Hannah Baby1, Elza John1
1. Dr. Noushad’s ENT Hospital & Research Centre*
ABSTRACT
Labyrinthitis Ossificans (LO) is the pathological ossification of the membranous labyrinthine spaces in response to an insult to the inner ear involving membranous labyrinth or the endosteum of the otic capsule.1 The pathogenesis of this condition is not well known. Earlier theories suggest that new bone formation could be metaplastic or osteoplastic. There are typically three phases of LO, acute, fibrotic and ossifying phase.2 The early identification of LO is important for hearing preservation, early intervention with possible cochlear implant placement, and alerting surgical colleagues to carefully evaluate obstruction during cochlear implant placement.3 Significant challenges related to the ability to place the cochlear implant arise with progression of LO and the extent of ossification throughout the membranous labyrinth, which may ultimately lead to alternative cochlear implant insertion techniques.4-5 Grade 2 labrynthine ossificans is the condition where a new bone or fibrous tissue replaces the 25-50% of the membranous labyrinth.
Here we report a case reported to us with the concern of hearing loss.
Keywords: Labrynthitis Ossificans, Cochlear implant, Modified Radical Mastoidectomy
Case description
A 68-year-old female reported to us with a concern of hearing loss in both ears. The patient is a known case of microtia in right ear. The patient has a history of left canal wall down surgery conducted 2 years back. Modified Radical Mastoidectomy (MRM) cavity present. The audiological evaluation was carried out. The results are as follows.
The pure tone audiometry results revealed bilateral profound mixed hearing loss. The patient was using hearing aid in left ear for 2 years. The aided discrimination was observed to be poor. The aided responses were out of speech spectrum. The patient was able to repeat 50% of phonetically balanced words.
The HRCT temporal bone plain imaging showed retracted tympanic membrane and absent ossicles, absent posterior and lateral semicircular canals in left ear. The MRI and HRCT of temporal bone with brain showed mictrotia in right ear with stenosed External Auditory Canal (EAC), non- visualized stapes, sclerosing mastoiditis and tegmen erosion. The left ear showed absent posterior and lateral semicircular canals and ossicles with grade 2 labyrinthitis ossificans of basal turn and postsurgical changes. No significant abnormalities were detected in brain.
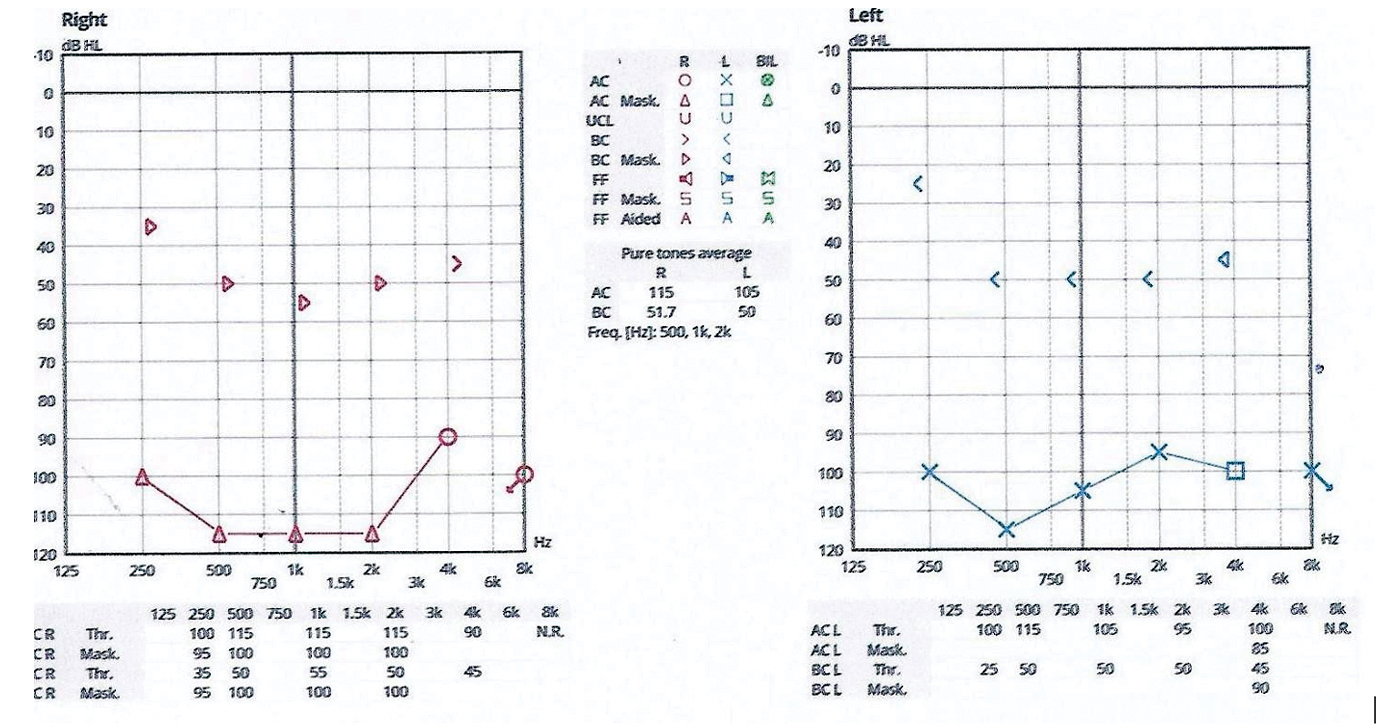
Figure 1. Represents the Pure Tone Audiometry results
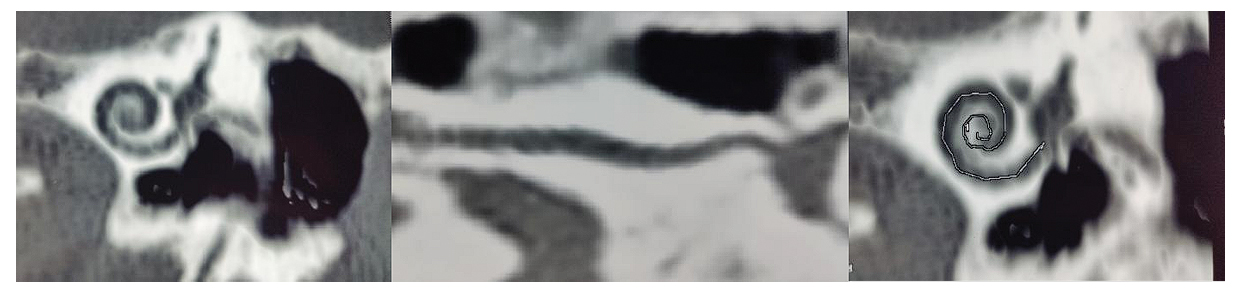
Figure 2. HRCT Temporal bone showing Grade II Labyrinthitis Ossificans, left ear [Thomas Balkany Classification]
Considering the deteriorating hearing of the patient cochlear implantation surgery was planned in the left ear. Under general anesthesia extended postaural incision was made and anteriorly based periosteal flap was elevated. Posterioinferiorly based musculoperiosteal flap was also elevated. Abdominal fat was harvested. MRM Cavity was seen. All accessible air cells were exenterated.
All mucosa from the middle ear cleft along with the tympanic membrane was removed. The round window was not identified. The extensive labrynthitis ossificans was seen. 8 to 9 mm of basal turn of the cochlea was drilled out and lumen was identified. The cochlear depth gauge was used to determine patency of the lumen and insertion depth. The well for receiver stimulator was made and the complete insertion of Cochlear CI 522 implant was done. The eustachian tube was closed with bone wax, muscle fat and surgicel. Receiver stimulator was fixed and the anterior flap was repositioned. The middle ear cleft was filled completely with fat and musculo periosteal flap. The circumferential elevation of external auditory canal was done. The blind sac closure was done and incision was sutured in layers.
The intraoperative measures were carried out to determine the integrity of the implant and the electrode array. The measurement revealed good impedance values. The neural response telemetry was carried out and obtained good neural responses across all 21 electrodes, except the first electrode. The switch on of the device was carried out after 12 days of surgery with Nucleus 7S sound processor. Similar results were obtained during post-operative impedance and neural response telemetry measures. The patient was able to appreciate speech sounds, would require extensive auditory training for better speech perception.
Conclusion
The preoperative measures help the surgeon to identify and predict the presence and extent of ossification or fibrous obstruction. Labyrinthitis ossificans, once considered a contraindication to cochlear implantation, can now be managed with specific surgical techniques yielding adequate overall hearing results.6 Along with cochlear implantation surgery, we also aimed at arresting recurrence of middle ear infections.
END NOTES
Author information
- Dr. Muhammad Noushad, Chief ENT & implant surgeon, Dr. Noushad’s ENT Hospital & Research Centre
- Dr. Vinay Thampuran P, ENT Surgeon, Dr. Noushad’s ENT Hospital & Research Centre
- Hannah Baby, Audiologist and Implant specialist, Dr. Noushad’s ENT Hospital & Research Centre
- Elza Joh, Audiologist, Dr. Noushad’s ENT Hospital & Research Centre
Conflicts of Interest: None declared.
Financial Support: Nil.
References
- Pritee Taxak, Chithra Ram. Labyrinthitis and Labyrinthitis Ossificans - A case report and review of the literature. J Radiol Case Rep. 2020 May; 14(5): 1–6.
[Pubmed] - H-Y Lin, Y-K Fan, K-C Wu, M-T Shu, C-C Yang,H-C Lin. The incidence of tympanogenic labyrinthitis ossificans. J Laryngol Otol.2014 Jul;128(7):618-20.
[Pubmed] - Trimble K, Blaser S, James AL, et al. Computed tomography and/or magnetic resonance imaging before pediatric cochlear implantation? Developing an investigative strategy. Otol Neurotol 2007;28: 317–24 CrossRef Medline
[Pubmed] - El-Kashlan, Ashbaugh C, Zwolan T, et al. Cochlear implantation in prelingually deaf children with ossified cochleae. Otol Neurotol 2003;24:596 –600 CrossRef Medline
[Pubmed] - Isaacson B, Booth T, Kutz JW Jr, et al. Labyrinthitis ossificans: how accurate is MRI in predicting cochlear obstruction? Otolaryngol Head Neck Surg 2009;140:692–96
[Pubmed] - Marc H. Hohman, MD,Douglas D. Backous, MD, FACS. Techniques for cochlear implant electrode placement in the ossified cochlea. 2010; Volume 21, Issue 4P239-242