Case Report Published on December 28, 2024
Unveiling the Intruder: Multiple Myeloma Presenting in Oral cavity
Vidya Aravind, Darshana Ravindran, Santhi T
1. Government TD Medical college, Alappuzha, Kerala*
ABSTRACT
Multiple myeloma is a common haematological malignancy, with varied presentations. A rare type of oral presentation of this disease, for which a series of investigations were needed to arrive at a diagnosis, is reported in this article. The aim of this report is to highlight the importance of carefully surveying the oral cavity for suspicious lesions, in order to avoid misdiagnosis and treatment delays. The clinical features and treatment modalities of multiple myeloma are also reviewed in detail.
Keywords: Multiple Myeloma, Oral Manifestations, Plasma Cell Neoplasm.
INTRODUCTION
Plasma cell neoplasms constitute 10% of all hematologic malignancies.1 These are characterised by atypical plasma cells with production of monoclonal immunoglobulins. Most common age of presentation is around 50 years with a male preponderance.1
Depending on plasma cell load and site of involvement, plasma cell dyscrasia is classified into monoclonal gammopathy of undetermined significance, extramedullary plasmacytoma and solitary plasmacytoma of bone.2
This case report describes a 60 year old female with history of a swelling in the gingivobuccal sulcus, which on investigation was diagnosed as Multiple myeloma.
CASE REPORT
A 60 year old female presented to the department with chief complaints of pain and swelling over the left gingivobuccal sulcus of 8 months duration. It was associated with generalized myalgia and backache for 5 months. She also had complaints of upper gingival pain and loose molar teeth with an absent second molar. The swelling gradually extended to the left premaxillary area. She had a medical history of diabetes mellitus, hypertension, hypothyroidism, dyslipidaemia and coronary artery disease.

Figure 1. Clinical examination
On intra oral examination (Figure 1), a firm swelling was noted over the left upper gingivobuccal sulcus with obliteration of the sulcus over the palatal root of second upper molar. A diffuse maxillary area swelling seen below the infraorbital. region of face, which was, tender to palpation, and firm in consistency with no local rise of temperature or discharging sinuses.
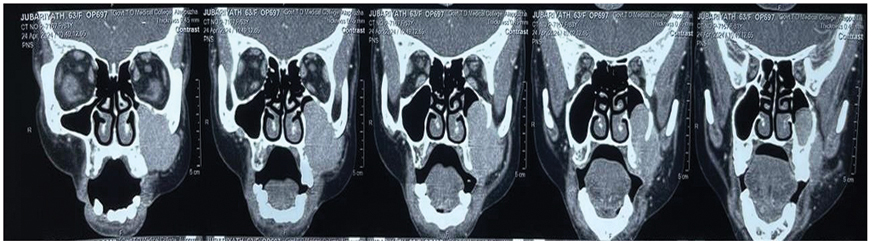
Figure 2. CECT nose& PNS
Initial radiographic evaluation with a cone beam CT scan suggested differential diagnoses of infected residual cyst, malignancy of maxillary sinus or periapical abscess. Contrast enhanced CT (Figure 2) scan of nose and PNS suggested malignancy maxillary sinus with bone metastasis or multiple myeloma, in view of the multiple lytic lesions noted over calvarium, maxilla, mandible and sphenoid along with the ill-defined heterogenous expansile lesion in the maxillary sinus.

Figure 3. X-ray showing lytic lesions
Multiple myeloma work up was done. Even though there was bony lytic lesions (Figure 3) in X-rays and anaemia, urine Bence Jones protein and serum electrophoresis were negative. Initial biopsy and histopathology done at a peripheral hospital was inconclusive
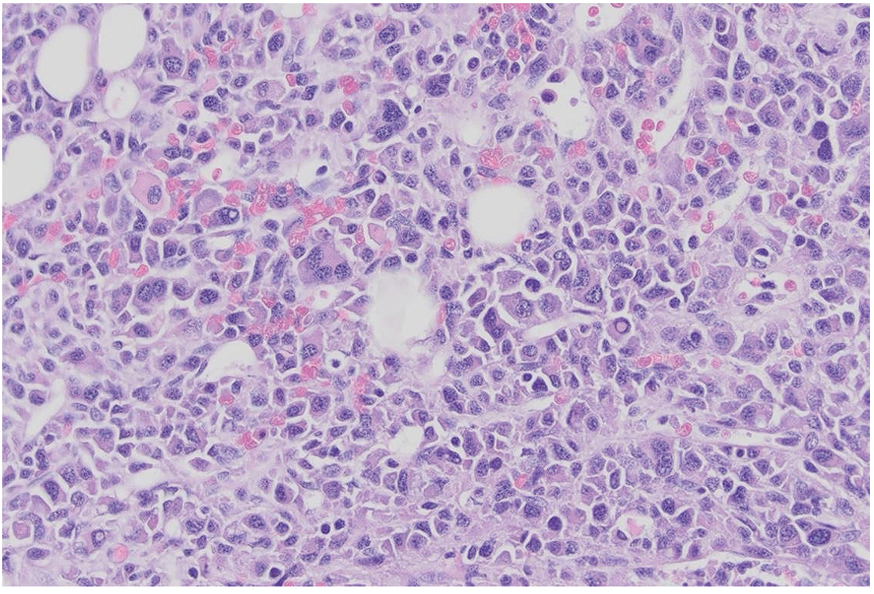
Figure 4. Histopathology
FNAC through gingivobuccal sulcus showed sheets of plasma cells, and a histopathology report of Plasmacytoma (Figure 4) was made with nasal endoscopic tissue biopsy from maxillary sinus with positive kappa neoplastic cells and positive CD 138. A Bone marrow biopsy revealed 30% plasma cells confirming the diagnosis of Multiple myeloma.
The Patient took treatment with chemotherapy, radiotherapy and plasma cell transfusion. She developed deep vein thrombosis during the treatment and expired after 3 months.
DISCUSSION
Multiple myeloma is a lymphoproliferative systemic disease of blood, with uncontrolled proliferation of monoclonal plasma cells in the bone marrow.2 The maturation stage of lymphocytes leads to production of abnormal plasma cells, which release immunoglobulins of uniform type, thus releasing M protein or paraprotein in the blood and urine. Sometimes, instead of the whole immunoglobulins, only light chains called Bence Johns proteins are released.3 The Bone marrow is the centre of blood cell production. These active sites of bone marrow are noted in pelvis, shoulder bones, spine, ribs and skull. Plasmacytoma usually develop in these areas.
The aetiology includes anything that interferes with the immune system including infection with cancer causing viruses. Toxic chemicals like benzene, dioxins, solvents, fuels and engine exhaust are identified as trigger factors. Viruses that have been implicated are HIV, herpes virus and simian virus.4 There can be generalized symptoms like mental confusion, bone pain, fatigue, neuropathy and susceptibility to infection. The localized region specific symptoms may be examined further to reach a conclusion.
Oral manifestations of multiple myeloma have an incidence of 2%-70%, in which jaw involvement is around 30% and can present as the first sign of the disease. Bony lesions are less common in the maxilla than in the mandible because of the lower amount of hemopoietic marrow.5 The median time from the onset of symptoms to the Multiple myeloma diagnosis is of 4–6 months. Multiple myeloma patients present with largely unspecific symptoms, such as back or skeletal pain, fatigue, prolonged infections, and deteriorating performance status. This may complicate initial diagnosis, since more frequently occurring differential diagnoses are considered, which induce similar symptoms.6
Diagnosis of multiple myeloma is by ≥10% clonal bone marrow plasma cells or a biopsy proven plasmacytoma with evidence of one or more multiple myeloma defining events (MDE): CRAB (hypercalcemia, renal failure, anaemia, or lytic bone lesions), bone marrow clonal plasmacytosis ≥60%, serum involved/ uninvolved free light chain (FLC) ratio ≥100 (provided involved FLC is ≥100 mg/L and urine monoclonal protein is ≥200 mg/24 h), or >1 focal lesion on magnetic resonance imaging.7
The treatment goal of the patient depends on the performance status of the patient, age, occupation, other comorbidities, candidacy for stem cell transplant, speed of response. The patients can be classified on the stem cell transplant recipients and not receipients of stem cell transplant. The Disease-specific therapy includes initial consolidation with high- dose chemotherapy and autologous hematopoietic stem cell transplantation, maintenance therapy, salvage therapy and supportive care includes management of hypercalcemia, skeletal complications, anaemia, infections and pain.8
Patients who are fit for transplant typically receive induction therapy over 3 or 4 months to decrease the tumour burden. This is followed by peripheral blood stem cell mobilization and harvesting and then an autologous stem cell transplant (ASCT), which improve the overall progression-free survival. The ASCT can be performed early after recovery from stem cell collection or it may be administered at the time of the relapse. After completing ASCT, the patient will be placed back on to a maintenance therapy till disease progression or intolerance to treatment.
In general, for those who are at high-risk and transplant eligible, induction therapy can be started with four cycles of daratumumab, bortezomib, lenalidomide, and dexamethasone followed by an early ASCT. After completion of ASCT, proteasome inhibitor-based maintenance therapy should be initiated and continued.
In those patients with standard-risk disease and transplant eligible, a similar algorithm is followed with a different drug regimen being used. Typically, induction therapy with four cycles of bortezomib, lenalidomide, and dexamethasone (VRd) is completed, followed by ASCT and then maintenance therapy with lenalidomide until disease progression or as tolerability permits.
For high-risk transplant-ineligible patients, there are several options. One approach would be to employ the VRd regimen for 8 to 12 cycles followed by maintenance bortezomib-based therapy.
For standard risk transplant-ineligible patients, options include VRd for 8 to 12 cycles followed by lenalidomide maintenance, or DRd (daratumumab, lenalidomide, and dexamethasone) continued until disease progression.9
This was an unusual case of multiple myeloma as she was an elderly female with prolonged history with swelling over the left maxillary sinus. There can be multiple differential diagnoses to the presentations similar to multiple myeloma. Hence a battery of tests may be needed to reach a definite diagnosis. Early detection can aid in avoiding complications and disease spread.
END NOTES
Author information
- Dr. Vidya Aravind, Junior Resident in ENT, Government TD Medical college, Alappuzha.
- Dr. Darshana Ravindran, Assistant Professor of ENT, Government TD Medical college, Alappuzha.
- Dr. Santhi T, Professor (HOD) of ENT, Govt TD Medical college, Alappuzha.
Conflicts of Interest: None declared.
Financial Support: Nil
REFERENCES
- Kyle RA, Rajkumar SV. Multiple myeloma. Blood. 2008 Mar 15; 111(6): 2962–72.
[Pubmed] - Kamath P, Babu C, Tamgadge A, Pereira T. Multiple myeloma with presentation in the oral cavity. J Oral Maxillofac Pathol JOMFP. 2022 Mar; 26(1):104.
[Pubmed] | [Crossref] - Cancer CCS/ S canadienne du. Canadian Cancer Society. [cited 2024 Oct 3]. The plasma cells.
[Source] - Issuu.com [Internet]. [cited 2024 Oct 3]. Patient Handbook.
[Source] - Ramaiah KKK, Joshi V, Thayi SR, Sathyanarayana P, Patil P, Ahmed Z. Multiple myeloma presenting with a maxillary lesion as the first sign. Imaging Sci Dent. 2015 Mar;45(1):5
[Pubmed] - Graziani G, Herget GW, Ihorst G, Zeissig M, Chaidos A, Auner HW, et al. Time from first symptom onset to the final diagnosis of multiple myeloma (MM) – possible risks and future solutions: retrospective and prospective ‘Deutsche Studiengruppe MM’ (DSMM) and ‘European Myeloma Network’ (EMN) analysis. Leuk Lymphoma. 2020 Mar 20;61(4):875–86.
[Pubmed] | [Crosref] - Rajkumar SV. Multiple myeloma: 2024 update on diagnosis, risk- stratification, and management. Am J Hematol. 2024 Sep; 99(9): 1802–24.
[Pubmed]| [Crossref] - Singhal S, Mehta J. Multiple myeloma. Clin J Am Soc Nephrol CJASN. 2006 Nov;1(6):1322–30.
[Pubmed] | [Crossref] - Multiple Myeloma Treatments | Drugs & Treatment by Stage [Internet]. MMRF. [cited 2024 Oct 3].
[Source]