Review Article Published on December 30, 2022
A Beginners Guide to Approaching a Patient
with a Perforated Tympanic Membrane
Manoj Manikoth1
1. Consultant Otologist and Cochlear Implant Surgeon, Dr Manoj’s ENT Institute, Calicut*
ABSTRACT
Perforations of the tympanic membrane are among the most everyday presentations to an otolaryngologist. Whilst many heal without treatment, there are some which need surgical closure. There have been so many ways to do this, and overall can be bewildering to a young Otologist. The article summarizes the most pertinent do’s and don’t’s to achieve a good result and how to maintain that over the years. The article is the result of many years work of by the author, a busy practising otologist for the last three decades.
Tympanic membrane perforations are common findings in an Otolaryngology outpatient. Patients present with complaints of discharge, hearing loss, tinnitus, inability to indulge in watersports, pain and sometimes difficulty in getting jobs. Fortunately, most acute perforations heal, but most chronic ones do not.1 The ear surgeon who comes face-to-face with an eardrum perforation is sometimes overwhelmed by the options in front of him/her. It is often desirable to have a structured protocol when dealing with such a condition. In the following few pages, we will deal with situations where the perforation has been around for a few months and show no apparent sign of healing. The topic deals with just tympanic membrane perforations; retractions and ossicular reconstructions are eliminated for brevity.
Rule 1. There is no guarantee that a small perforation will heal and that a large perforation would not
However skilled or experienced the Otolaryngologist may be, the perforation sometimes behaves in very strange ways. A small perforation may linger on with repeated ear discharge and pain. In contrast, what appears like a large perforation that needs surgery sometimes heals inexplicably. What then, is the time frame when you decide to do surgery or not? Most people believe that a perforation that does not heal in six months has a very low chance of healing. What then would you do to help that process? The author prefers inactivity. Keeping the ear dry during bathing with a pledget of cotton wool smeared generously with white petroleum jelly and treating allergic episodes promptly may help to keep the mucosa healthy. It is debated whether you apply antibiotic or antibacterial eardrops in a perforation2 (Figure 1).
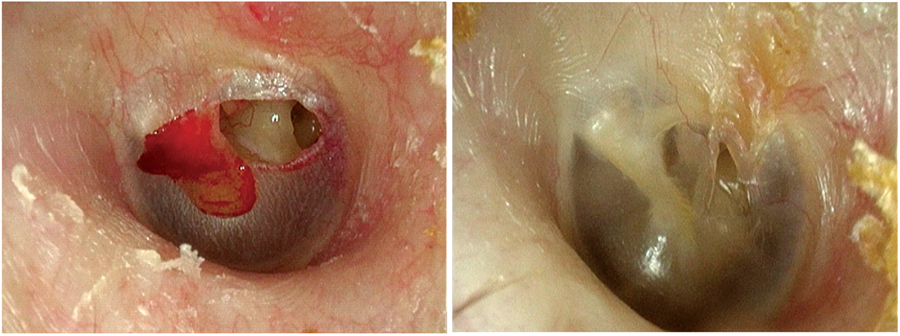
Figure 1. Perforation healing with just observation – 6 months
Those who are in favour of eardrops claim that the concentration of antibiotics locally exceeds by many times what you can give orally or parenterally. However, most ear drops are acidic and may cause pain on instillation and may cauterize the edges of the perforation and make it larger. If a perforation is just moist and not discharging, it is quite prudent not to instill anything. Most patients complain of severe discomfort when ear drops are applied to the naked middle ear mucosa. Oral antibiotic therapy does no change to an inactive chronic perforation. Neither do antihistamines or decongestants. Careful suctioning under the microscope without causing discomfort is the best method to get the ear dry. It may be difficult in very young children, but in most others, it is quite effective in avoiding most medical treatments.
It has been the practice in our centre to watch a perforation over several months with audiograms to see if there is any sign of healing if the duration is not known or if the patient is sure, it is recent. Decreasing hearing or repeated discharge would mean that surgical intervention would be the best method of intervention. In general, 35dB or less of conductive hearing loss would not cause much discomfort to the patient. Anything more, a surgical method to close the perforation and reduce the risk of reinfection would be more prudent.
Rule 2: a wet perforation is no contraindication to surgery
For a long time, there has been overwhelming evidence that tympanoplasty surgery in both wet ears and dry ears does not have different outcomes. People like us who regularly and for a long time operate on wet ears find that surgery is not difficult in wet ears, but in fact, is easier because the demarcation between healthy and diseased parts of the eardrum is more pronounced in wet ears. However, it has been taught, without any evidence to support it, that wet ears have poorer graft take-up. The distraught surgeon often spends a long time to get the ear dry before surgery and when failures happen, is left wondering why. Sometimes the smallest of all perforations may have the most profuse discharge, and the large ones remain relatively dry. Shambaugh, in his book, had mentioned that “a surgeon should never hesitate to make a small perforation larger if that would help proper graft placement “. A large study by Mario Sanna proved that graft take-up was better in wet ears. I personally have been operating on both wet and dry ears and do not believe that the graft take-up is any different. If that were the case, what does one benefit from giving antibiotics to get an ear dry? (Figure 2 & 3)

Figure 2. Pre-Operative

Figure 3. Post-operative- 6 weeks, myringoplasty in a wet ear
Rule 3: Culture sensitivity of the discharge is of no value whatsoever
Taking a swab of the discharge from the ear canal is of no value in Chronic Otitis Media. There is value, however, in cases like Skull base Osteomyelitis and in certain cases of Acute otitis media where the culture is taken by aspirating through the TM without contaminating, so culturing the bacteria in a wet ear would only make you start an antibiotic that you can very well do without.
Rule 4: the canal decides the approach, and so does the surgeon’s experience
The question in every young surgeon’s mind is how to approach the patient. Would you do a transcanal procedure; or would an endaural suffice? Would you rather use the post-aural approach? The honest answer is – it does not matter. A large canal where you see every part of the Tympanic Membrane would be ideal for a transcanal procedure, but people must understand that the surgical expertise needed for this is considerably high (Figure 4). The post-aural approach is easy and straightforward. It does not take much more time than transcanal surgery. There is a risk of wound infection, of course, but that can be prevented by simple adherence to sterile techniques. As one gets older and wiser, maybe all approaches can be done with equal finesse and flair, but one must never get into a trap of a patient wanting to do surgery a particular way and yielding to that temptation knowing well that one’s ability does not match the procedure. Patients can choose if surgery must be done or not, but how it is to be done is the surgeon’s prerogative. One must never forget that.
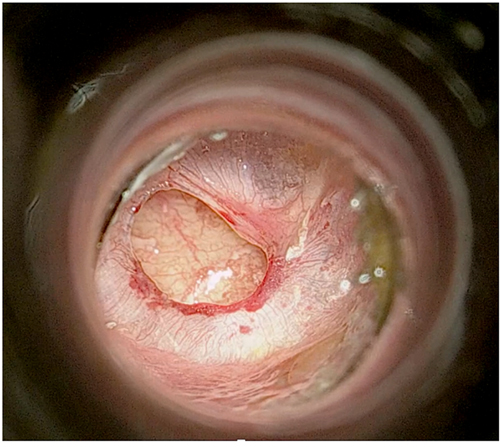
Figure 4. A typical transcanal myringoplasty scenario
Rule 5: Canaloplasty works- all the time
Widening the canal for proper visualization of the entire tympanic membrane is purported to have many advantages.3 They are (a) proper placement of graft 360 degrees (b) increased blood supply to the graft by opening the Haversian canal system (c) better hearing due to increased resonance of the wider external canal. However, only the first is a logical argument and the other two have never been proven beyond doubt. Canaloplasty is far from safe, however. You can damage the skin of the external canal, create a mastoid canal fistula, tear the annulus off, and cause acoustic damage to the ossicular chain by inadvertently touching it with the burr. You can minimize these dangers by carefully elevating the entire skin of the external canal with the periosteum before doing the canaloplasty, by keeping a disc-shaped piece of silastic or aluminium foil and by being very careful close to the annulus. It takes time to learn proper canaloplasty. Ideally, you need to start in the posteroinferior quadrant, move on to the floor and then the anterior half. The area superior to the tympanomastoid suture line is dangerous because of the proximity of the mastoid air cells and may be the reason for persistent discharge even if the drum heals perfectly (Figure 5).

Figure 5. Canaloplasty- start inferior and protect canal skin at all times
Rule 6. Perichondrium, facia, or scar tissue- all grafts are the same
The argument of which is the better graft has gone on forever. But the conscientious surgeon knows that there is no “ideal” graft. How you place it is more important than what graft it is. The graft should be thin, easily placed, adequately sized and without holes in it. The author has been using various grafts with the same results. In transcanal and endaural procedures we prefer the tragal perichondrium. For post-aural procedures, we use the post-aural periosteum, temporalis fascia or scar tissue if it is a revision. Facia Lata is sometimes taken when a large graft is needed. The graft is just a substrate for the epithelium to grow on. Giving more meaning to it is futile You can however bolster it with some cartilage if you think you need to prevent a retraction (Figure 6-9).

Figure 6. Tragal perichondrium Harvest
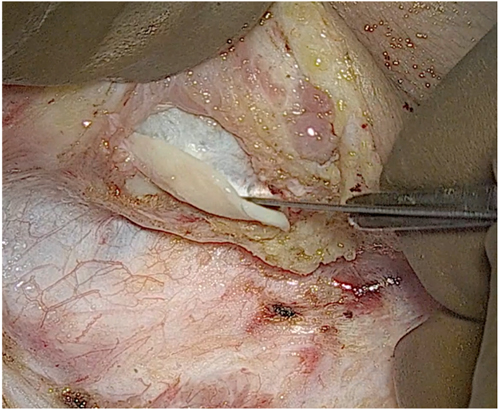
Figure 7. Tragal perichondrium Harvest
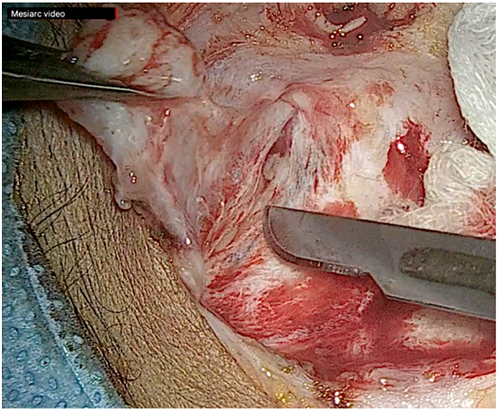
Figure 8. Temporalis fascia Harvest

Figure 9. Facia lata harvest from thigh
Rule 7. The technique of graft placement of Interlay tympanoplasty
All of us who have been operating on ears with perforations for a long time know that we have all evolved. There is a slow and gradual climb up to acceptable success rates and long-term good results. Personally, I have found interlay tympanoplasty to be the most reliable of all techniques in tympanoplasty. Gradually exposing the annulus after doing a wide canaloplasty if necessary, careful dissection under the annulus and removing all the fibrous layers away from the mucosa, elevating the remnant 360 degrees and placing the graft over the mucosa and relaying the elevated portion is not only easy to do but bypasses two of the most difficult steps in tympanoplasty – the freshening of the edges and the anterior tuck of the graft (Figure 10). The graft heals quickly and completely and post-operative mucosalisation is surprisingly low. Watching a few surgeries and a little diligence and dexterity is all that is needed to learn this good technique.

Figure 10. Graft placement- interlay. Before and after (right)
Rule 8. A cortical mastoidectomy is unnecessary, even for wet ears
For a long time, a cortical mastoidectomy was done to reduce failures and to eliminate the mastoid reservoir with scarcely any evidence of benefit for both these reasons. Research and meta-analysis have proven conclusively that mastoidectomy gives no added benefit to a well-done tympanoplasty. Moreover, mastoidectomy is the cause of most of the complications following tympanoplasty- facial nerve injury, labyrinthine injury, mastoid canal fistula, sigmoid sinus bleed, Dural injury and herniation, CSF leak and ossicular damage. If the same results are available without mastoidectomy, would it not be foolhardy to add this part of the surgery that is fraught with all those risks? I am not claiming that I have never done a mastoidectomy as a part of tympanoplasty; in contrast, we were doing it for most wet ears. I knew that this was not supported with evidence, but sometimes it is hard to break a habit. Then COVID came and the fear of aerosol spread during mastoidectomy gave us an excellent opportunity for doing all cases without a mastoidectomy and to evaluate the results. The result was just as I thought it would be -there was absolutely no difference in our results. The conviction I had finally had its logical conclusion.
Rule 9. The importance of audiologic evaluation, before and after
The hallmark of every surgery is the long-term result. Proper pre- and post-op evaluation of hearing is the key to patient satisfaction and improving one’s own results. Sadly, though most people do a pre-operative audiogram, very rarely do you see serially done post-operative audiograms in this country. Ideally, a pre-operative audiogram must have both air-conduction and bone-conduction thresholds marked, and speech audiometry performed. After the surgery, the post-operative testing is done at six weeks, six months, and 2 years after surgery in most cases. One should never fear a less-than-optimum or a bad result. It shows honesty on your part as a surgeon and helps you iron out your mistakes and find out what you can do better (Figure 11-14).

Figure 11. Pre-operative audiogram
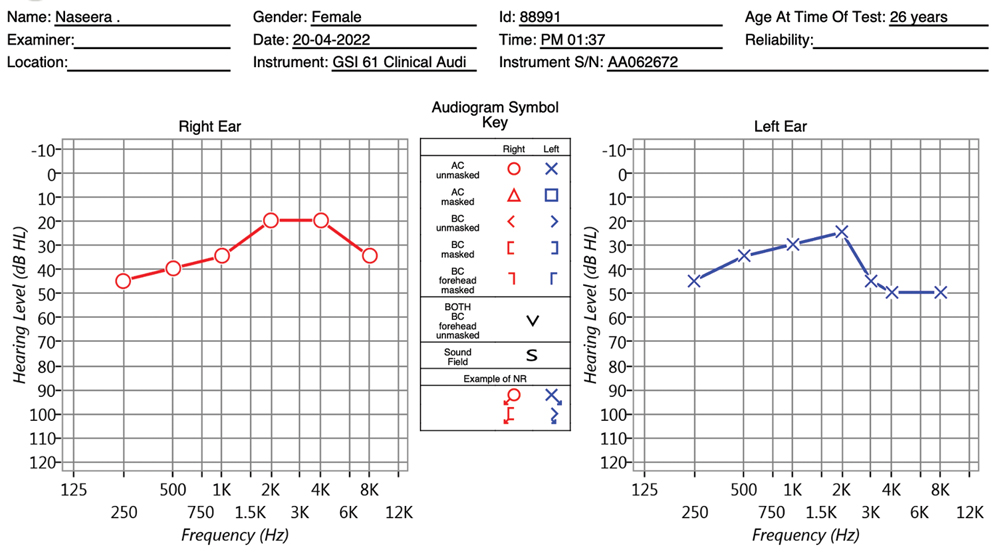
Figure 12. Immediate post- operative

Figure 13. 2-year post-operative
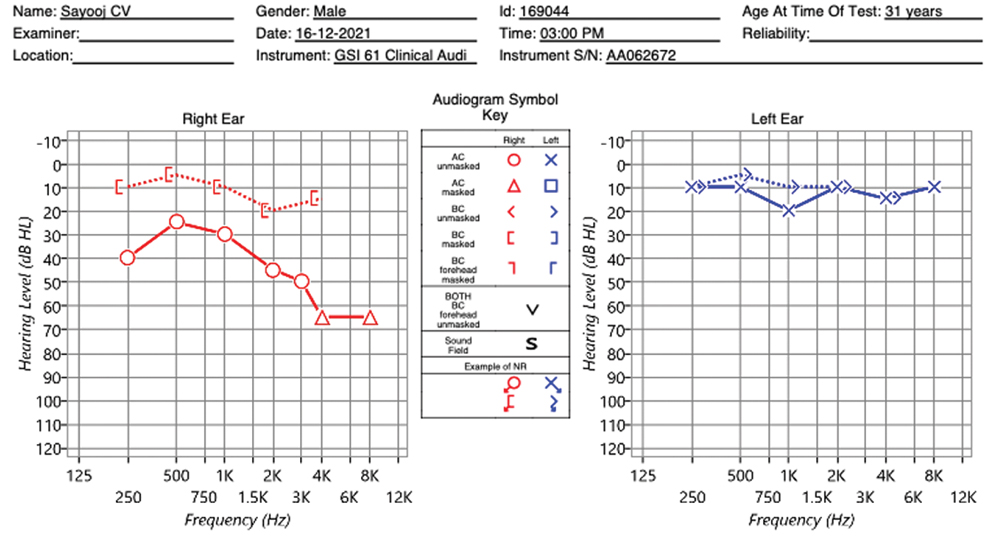
Figure 14. 7-year post- operative
Rule 10. Post-operative care must be always under the microscope
Every visit post-operatively must be examined under a microscope. Seeing a possible failure, clearing out debris or cauterizing a small canal granulation are all better done with an outpatient otologic microscope. One should never ignore this important step. A small area of pulsatile discharge should make one suspect early graft dehiscence- maybe adding an appropriate antibiotic then would promote healing. A small area of granulation tissue may respond quickly to cauterization. Gentle suctioning with a 22 suction will remove debris without damaging the graft
Rule 11. The grace of accepting a failure
Grafts fail. That is a universal truth. How you handle it is very important. A graft failure is evident by the sixth week itself (Figure 15). It is important to tell the patient that there is a problem and reassure them that whatever the outcome, it will be managed. The importance of group practice is to be emphasized here. Especially if you are young and inexperienced, and if there is a senior colleague, it is important to get his or her help to manage the failure. However, it is ethical practice to help correct this failure with as little discomfort as possible for the patient. A graft failure needs to be corrected only after 6 months. An earlier attempt at reconstruction is not only unnecessary but also difficult and not safe for the patient.4
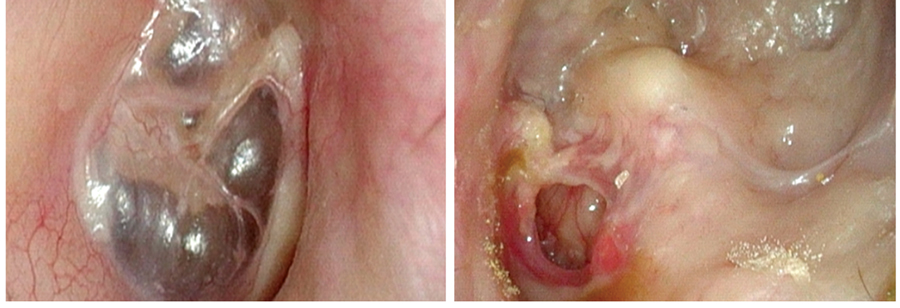
Figure 15. Graft Failure in an otherwise well-done Mastoidectomy – left ear.
The operating surgeon must be the first one to disclose the failure to the patient; it is not wise to let them hear from anyone else. A small pinhole perforation, less than 1mm, if dry need not be closed- it will hardly create an issue. A well-taken-up graft, but poor hearing is another issue. The cause could be as simple as a missed ossicular erosion or fixation, or more ominously, a sensorineural hearing loss. These are preventable complications but, nevertheless.
End Note
Author Information
- Dr Manoj MP . MS ( ENT) Consultant and Head of Department of Otology Neurotology, Dr Manojs ENT Institute, Calicut, Kerala, India 673005
Conflict of Interest: None declared
References
1. Gladstone HB, Jackler RK, Varav K. Tympanic membrane wound healing. An overview. Otolaryngol Clin North Am. 1995 Oct;28(5):913–32.
[Pubmed]
2. Roland PS, DoharJE, Lanier BJ, et al. Ciprofloxacin/dexametha- sone versus ofloxacin for granulation tissue in AOMT patients. Presented at the annual meeting of the American Academy of Otolaryngology-Head and Neck Surgery; Sept. 22, 2003
3. Parisier SC, Levenson MJ, Hanson MB. Canalplasty. Otolaryngologic Clinics of North America. 1996 Oct 1;29(5):867–86.
[Source]
4. Shelton C, Sheehy JL. Tympanoplasty: review of 400 staged cases. Laryngoscope. 1990 Jul;100(7):679–81.
[Crossref] | [Pubmed]