Case Report Published on June 20, 2024
Migration Beyond Imagination - A Case Report
Bonny Thomas P1, Ramesh Kumar E1
1. Department of Otorhinolaryngology, Jubilee Mission Medical College and Research Institute , Thrissur, Kerala*
ABSTRACT
Coins, bones, food bolus etc. are some of the common foreign bodies that can get impacted in the throat.1 At times there may be some usual foreign bodies that can get impacted in some unusual sites.1 The main aim and objective of this report is to highlight on foreign body impaction in the unusual site. We present the case report of a patient who accidentally dodged a foreign body at an unusual site.
Keywords: Usual foreign bodies, Unusual sites
Introduction
Foreign bodies can present a diagnostic challenge sometimes even to the experienced surgeon. In one review of 200 surgical cases involving retained foreign bodies, one-third of the cases had been initially missed. We present an interesting case of a foreign body- fish bone in the parotid gland.
Case presentation
34 year old male patient, known case of Diabetes mellitus, pancreatitis presented with complaints of foreign body (fish bone) cheek right side, of one day duration. Associated with mild neck pain. No complaints of difficulty in swallowing.
Patient, who has been working as a cook, presented to the OPD with 1 day history of fish bone in the cheek right side. On detailed examination no foreign body could be visualised in the oral cavity or oropharynx.
Videolaryngoscopic examination also did not show any foreign body in the hypopharynx.
Patient was sent off with antibiotics and analgesics in view of his diabetic status. Two days later patient presented with slightly increased pain, but this time he was pointing over the right parotid region more, than inside the cheek.
On examination patient had slight redness and tenderness over the right parotid region. The patient’s body temperature, respiratory rate, blood pressure, and heart rate were all within normal range. He had elevated blood sugars ranging 300 – 400 mg/dl, which was controlled later. All other blood parameters were within normal range.
The patient had undergone CT evaluation neck. Imaging results (Figure 1, Figure 2) revealed linear hyperdense structure measuring 25 x 2 mm noted lying horizontally in the superficial lobe of the right parotid gland, with acute inflammation around the foreign body.
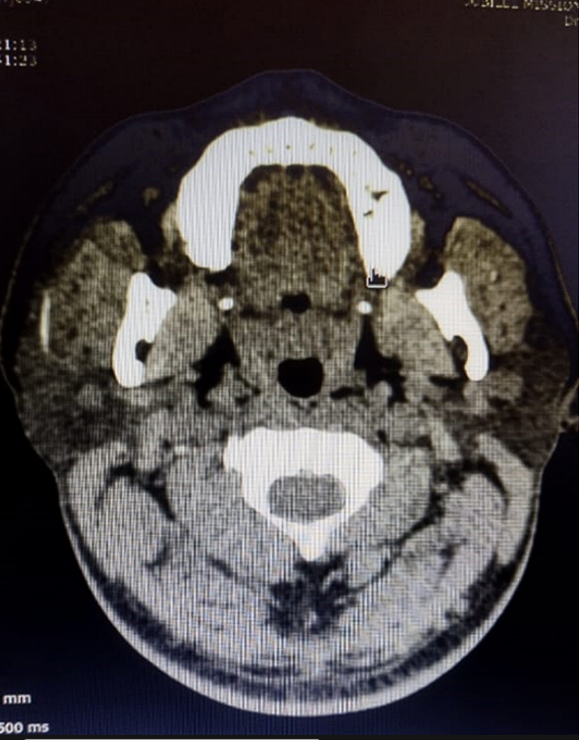
Figure 1. CT, axial cut across parotid gland , showing linear hyperdense structure
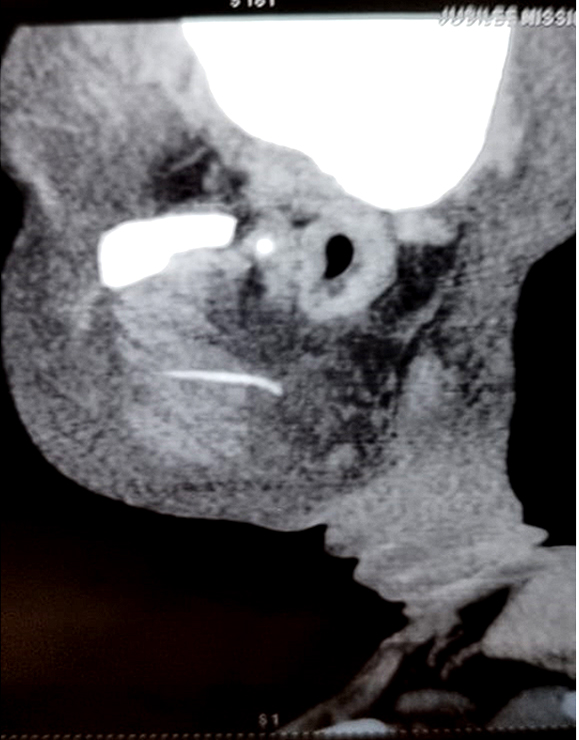
Figure 2. CT sagittal cut at parotid gland, showing linear hyperdense structure
Treatment and follow up
It has been decided to explore the parotid region for foreign body removal. The major concern of facial nerve injury was thoroughly discussed with the patient as it was his immediate prewedding days.
Under general anaesthesia and local infiltration with saline and adrenalin a vertical incision in front of the tragus like in classical parotidectomy but without extending to the mastoid tip, flaps raised above the parotid capsule which is further deepened into the superficial lobe of parotid tissue. Dissection continued parallel to the direction of facial nerve branches. As there was inflammation around the foreign body there was some bleeding while searching for the fish bone.
Finally the fish bone (Figure 3) was identified and removed, though it was not easy. No facial nerve injury at the end of the procedure.

Figure 3. Foreign body
Discussion
Complications associated with foreign bodies are rare; however, if migrated in the aerodigestive tract, they can cause significant morbidity and, in some cases, mortality.2 The majority of foreign bodies ingested pass through the digestive tract uneventfully.2
Unlike other foreign bodies, fish bones are sharp and have a propensity to perforate the aerodigestive tract. They are not inert and often harbour organisms, which easily predispose them to abscess formation.2
Perforating and migrating foreign bodies is much rarer. In 10 years, Al Sebeih et al. could only detect 11 patients in which the foreign body perforated the digestive tract and migrated to the neck space.3 The incidence of neck abscesses following foreign body ingestion has been assessed to be around 0.21% and 0.96% in two separate studies.3
The most common site at which a foreign body could perforate the oesophagus to become extraluminal is at the cricopharynx, which is the narrowest part of the oesophagus. Attempts under local anaesthetic, flexible endoscopes were the common causes of migration. Loh et al. studied 273 cases of foreign bodies in the oesophagus.4 They reported a major complication rate of 7.3% in their study.4 According to them, foreign body impaction increases the risk of perforation 14 times.4
Migration from upper oesophagus is most commonly seen into parapharyngeal and retropharyngeal spaces. Rarely migration into the nasopharynx is also seen - incorrect grasping and forceful attempts of removal are the causes of migration in this direction. Migration of mid oesophageal foreign bodies into the mediastinum is associated with high fatality rates.
In the presented case migration was very unique were the foreign body has transgressed through the buccal mucosa and the whole thickness of parotid gland to take a position in the superficial lobe of the gland and risking the facial nerve injury while removal.
In conclusion, foreign bodies, especially in an atypical location like the parotid gland, can be a diagnostic challenge. Thorough history taking complemented by appropriate imaging modality can help in prompt diagnosis, treatment and a complication-free recovery.
END NOTE
Author Information
- Dr. Bonny Thomas P, MBBS, Junior Resident
Department of Otorhinolaryngology,
Jubilee Mission Medical College and Research Institute, Thrissur, Kerala - Dr. Ramesh Kumar E, MS, DNB,
Associate Professor
Department of Otorhinolaryngology,
Jubilee Mission Medical College and Research Institute, Thrissur, Kerala
Funding Source: There was no funding from any external agency
Ethical Standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation (please name) and with the Helsinki Declaration of 1975, as revised in 2008.
Conflict of Interest: None to declare
References
- Opoku-Buabeng, J., & Abdulai, R. (2012). Unsual foreign body in the throat: a report on 3 cases. Journal of the West African College of Surgeons, 2(3), 88–95.
[Pubmed] - Hussain, S. Z. M., Kk, A., Mohammad, A. W., & Khan, M. (2022). Migratory Foreign Bodies in the Aerodigestive Tract: The Importance of CT Imaging. Cureus, 14(1), e21595.
[Pubmed] | [Crossref] - Mathew, R. P., Liang, T. I., Kabeer, A., Patel, V., & Low, G. (2021). Clinical presentation, diagnosis and management of aerodigestive tract foreign bodies in the paediatric population: Part 2. SA journal of radiology, 25(1), 2027.
[Pubmed] | [Crossref] - Sinha, R., Sen, I., Saha, J., Mukherjee, A., & Guha, R. (2013). Migration of a fish bone from the upper aerodigestive tract to the skin of the neck: a case report. Ear, nose, & throat journal, 92(8), E15.
[Crossref]