Case Report Published on June 20, 2024
Trans Nasal Endoscopic Choanoplasty- The Ideal
Treatment Option for Choanal Atresia and Stenosis
Sajith Babu Thavarool1, Manu Santosh2, Ram Guruprasad3, Janani Anandkumar1, Mihir Mohan1
1. Department of Head and Neck Surgery, Aster MIMS, North Kerala Cluster; 2. Department of Head and Neck Surgery, Aster MIMS, Kannur; 3. Department of Head and Neck Surgery, Aster MIMS, Calicut*
ABSTRACT
Here we present one patient with bilateral congenital atresia and two patients with acquired stenosis which were managed successfully with trans nasal endoscopic choanoplasty. Review of literatue of the history of the disease, its dagnostic methods, and treatment options are made. The evolution of surgery to the current trans nasal endoscopic choanoplasty is described.
Keywords: Choanal Atresia, Choanal Stenosis, Choanoplasty
Introduction
Choanal atresia (CA) is the condition in which the posterior choana is completely occluded by bone or membranous mucosa or a combination of both. Choanal stenosis (CS) is the condition in which there is partial occlusion of the posterior nasal choana. Choanal atresia or stenosis can be a congenital condition which occurs in about one in 5000 to one in 9000 live births. It can be either unilateral or bilateral and causes severe respiratory symptoms in the immediate neonatal period when it is bilateral.
Congenital stenosis may be asymptomatic till adulthood. Acquired stenosis may occur because of surgery, infection or radiation treatment which can be mild, moderate or severe.
Here, we describe a patient with bilateral congenital atresia and two patients of acquired stenosis which were managed successfully with trans nasal endoscopic choanoplasty.
Case Reports
Patient 1: Bilateral congenital choanal atresia (Figure 1)
A term male child with 2.23kg birth weight was referred from a peripheral hospital to the neonatology department on day 1. He had not cried soon after birth and there was a suspicion of bilateral choanal atresia. He was started on mechanical ventilation and imaging with CT nose and paranasal sinuses was performed which confirmed bilateral complete osseous choanal atresia. He was evaluated for other defects and was found to have coloboma of right eye, fossa ovalis ASD (4mm) and PDA (2.2 mm) with left to right shunt and severe pulmonary arterial hypertension. There were no other deformities or defects.
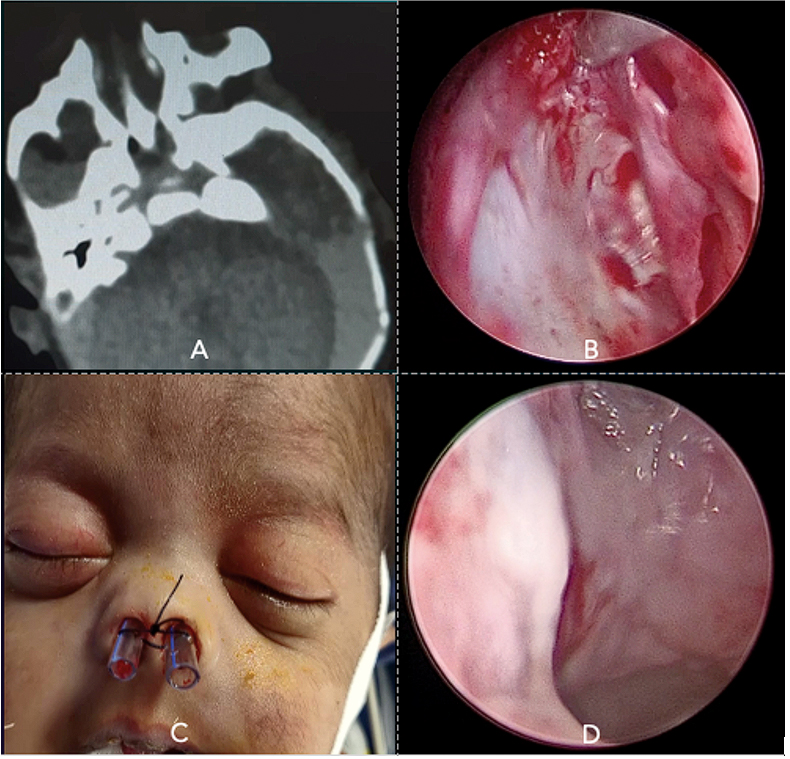
Figure 1. (A) CT scan of the neonate showing the bilateral bony atresia,
(B) Endoscopic picture of the neonate showing the complete stenosis on left side,
(C) Post operative picture of the neonate with the endotracheal tube as the stent,
(D) Endoscopic picture of the posterior choana after two weeks post operative period
He underwent bilateral choanal atresia repair (Choanoplasty) under GA on day 2. Intraoperatively, both choanae were found to be completely closed with thick atretic bone. The mucosa over the posterior most part of the septum was elevated on both sides and adjacent bony septum was excised. A midline defect was formed which acted as guide to nasopharynx and the atretic bone laterally was drilled and widened to adequate size. The child was extubated the following day and was put on high flow nasal oxygen which was subsequently tapered and stopped. A follow up nasal endoscopy after 2 weeks showed adhesions in posterior nasal cavities between septum and inferior turbinates. He underwent adhesionolysis followed by insertion of 3.5mm endotracheal tube as a stent with multiple small perforations to facilitate drainage of nasal secretions and prevent sinusitis. The tubes were secured with sutures anteriorly and removed after 14 days. Nasal endoscopy done at the end of two weeks showed a well healed and adequate sized choanae on both sides and the baby was breathing normally and feeding on breast milk without difficulty.
Patient 2: Bilateral acquired choanal stenosis with stenting
A 30-year-old female presented to the Head & Neck Surgery OPD with complaints of breathing difficulty and nasal obstruction in February 2024. There was no history of nasal discharge, nasal bleeding, or any ear-related symptoms. She was diagnosed with nasopharyngeal carcinoma (cT1N0) which was treated with chemoradiotherapy (70Gy/35#) in April 2022. On direct nasal endoscopy, a septal perforation with mild crusts and near total stenosis of the posterior choanae was noted. On palpation with the probe, the stenosis appeared to be fibrotic tissue. She underwent trans nasal endoscopic choanoplasty with stenting. The procedure involved removing the posterior nasal bony septum, resection of the hard fibrosed mucosa at the choana, and releasing adhesions bilaterally with monopolar suction cautery. A nasal stent using an endotracheal tube, cut at both ends and perforated for air passage was passed through the oropharynx into the nasal cavity looping around the posterior septal margin and secured anteriorly with a suture. On post operative day 14, the stent was removed, and crusts cleared and was initiated on nasal douche. Nasal endoscopy was repeated after two months and showed adequate opening of the choana.
Patient 3: Bilateral acquired choanal stenosis without stenting
A 33 year old lady with a history of carcinoma nasopharynx post radiotherapy in 2019, presented in 2022 with complaints of decreased hearing on both sides and persistent nasal blockage. She has a history of bilateral myringotomy and grommet insertion twice in the past.
She was evaluated with nasal endoscopy and was found to have stenosis of choanae on both sides with no evidence of recurrence. Pure tone audiometry revealed a conductive type moderate hearing loss with Type B tympanogram on both sides. In January 2022, under general anaesthesia posterior septectomy was done preserving mucoperiosteal flaps on both sides. Stenotic choana was widened with coblator and micro drill medially from both sides and made into a single wide opening. Mucosa and underlying soft tissue were excised laterally to completely visualise both eustachian tubes which were found to be anatomically normal. The preserved mucoperiosteal flaps were fashioned and interposed to posterosuperior aspect for adequate cover for exposed bone and was kept. Bilateral myringotomy and grommet insertion was done. On follow up after an year, her hearing was improved and the nasopharyngeal opening was patent.
Discussion
Adolph Wilhelm Otto published his finding of this condition in autopsies in the year 1831.1 Whereas various articles in the literature have mentioned that choanal atresia was first described by Johann George Roederer in 1755. Since then, there had been various reports of this condition even untill the current year.2
The overall prevalence rate of choanal atresia and stenosis is 0.92/10000 livebirths.3 There is a rule of two which states that CA is twice more common in females, twice on the right side and twice unilateral compared to bilateral.4 It is difficult to diagnose CA or CS in the antenatal period though rarely, it can be diagnosed on evaluation of polyhydramnios wherein there is absence of flow of amniotic fluid through the nostril.5 In the post-natal period, it can be suspected immediately because of respiratory distress or later due to nasal blockage. A bedside diagnosis can be made if few drops of saline instilled into the nose flows back or a catheter fails to pass through the nasal cavity.6 A suction catheter or red rubber catheter of size 6-8 Fr can be used. If the obstruction is felt 1-2cm from the nostril, it could be due to deviated nasal septum and if it is about 3-4 cm from the nostril, a stenosis or atresia can be suspected. A flexible endoscope or rigid nasal endoscope can be used further to evaluate the nasal passage. The other causes of obstructions like deviated nasal septum, mucus plug, enlarged turbinate, tumors, cysts etc. need to be ruled out.
Previously, X Rays with trans nasal dyes were used to confirm the diagnosis.7 The presence of bone and or membranous obstruction can now be confirmed by a computerized tomogram(CT).8 The posterior choana is formed by the sphenoid bone superiorly, vomer medially, pterygoid plate laterally and the palatine bone inferiorly. In atresia or stenosis, there is thickening of the vomer bone and the medial pterygoid plate. There can be medialization of the pterygoids in the computerized tomogram findings. If the posterior choana measures less than 3.4 mm in the maximum transverse distance and the vomer thickness is more than 5.5 mm, a diagnosis of choanal atresia can be made.9 The atresia can be purely bony in 29% of cases, mixed type with osseus-membranous in 71% and purely membranous in none.8 A CT scan will show other abnormalities in the skull as well.
The exact reason for development of CA/CS is not known. There are embryological models10 and molecular models. The embryological model suggests that it could be due to the failure of opening of the naso-buccal membrane or persistence of the bucco-pharyngeal membrane. The molecular model suggests that it could be due to dysfunctional vitamin A metabolism or use of carbimazole for hyperthyroidism.
About 50% of these patients may be associated with syndromes like CHARGE, Treacher Collins, Pfeiffer, Antley Bixler, Marshal Smith and Crouzon. The most common among this is the CHARGE syndrome which occurs in about 30% of the patients. The major criteria apart from CA, for the syndrome are ocular coloboma, external ear anomaly, cranial nerve palsies and minor criteria includes heart abnormalities, cleft lip/palate, facial malformation, developmental delay, hypoplasia of genitalia, trachea-oesophageal fistula and dysfunction of hypothalamo- hypophyseal system.11 All the neonates with confirmed unilateral of bilateral CA/CS should undergo screening for other abnormalities and need a cardiologist, neurologist and ophthalmologist consultation. Brainstem auditory evoked response should be done in all patients after the neonate stabilizing with the cardiac conditions. Inner ear abnormalities such as Mondini defect can be detected in the CT scan of the temporal bone.
The treatment is by surgical correction in symptomatic stenosis and in all atresia. Bilateral atresia is an emergent condition as they usually present with respiratory distress. The neonate usually requires endotracheal intubation in view of cyanosis immediately after birth. Further evaluation and treatment can be done in the intubated baby.
Trans nasal blind puncture with curved trocar, was described by Carl Emmert in 1854.12 Puncture followed by dilatation and stenting were followed as a safe procedure starting from Borse in 1907, until the advent of the endoscopes. Trans palatal surgeries were described as early as 1909 by Brunk and were continued till the 1980s.
Current treatment strategies include trans nasal endoscopic surgeries which were first described by Stankiewicz. Trans nasal surgeries are better than trans palatal surgeries as there are less chances of crossbite, high arch palate, palatal flap necrosis and fistula.13 One method is to puncture the posterior atretic plate if it is membraneous or of thin bones and then dilate it with drill and debrider. Other method is to remove the posterior bony vomer as well as the medial part of the pterygoid plates. In a meta-analysis, Durmaz et al found that trans nasal endoscopic surgeries have better success rate and lesser complications than other surgeries.14 Mucosal flaps may be raised in adults and then used for covering the raw bony surfaces. This helps in early healing and is believed to reduce stenosis.15 Stents may be used to prevent re stenosis and the common ways are to use modified endotracheal tube16 or self-diluting stents.17 M O Tomum et al. from Egypt did a randomized controlled trial, to study whether flaps and stents are useful in these surgeries and found that there was no difference in incidence of re stenosis in groups with and without stents. The mucosal flaps give good cover to the raw bones and prevents granulations whereas stents cause more granulation, columellar necrosis and discomfort.18 Otology instruments may be used for endoscopic choanal surgery in the neonates along with 2.8 or 4mm endoscopes. There are various adjuncts that can be used with endoscopic surgeries like LASER or application of mitomycin C, both of which has no definite advantages. CT/MRI based navigation may be used especially in patients with skull base malformations to guide the atretic plate.
The national recommendations for diagnosis and management formulated by the Slovenian Medical Association for the diagnosis and treatment of CA6 suggests that bilateral CA in a neonate should be treated between 10th and 13th day even in case of premature birth. They also recommend trans nasal endoscopic surgery in all possible patients and puncture and stenting should be done only if nasal cavity is very small. The child should be followed up for at least two years, to look for re stenosis and re surgery if necessary.
Conclusion
Here, we present case reports of three patients with congenital bilateral choanal atresia, acquired bilateral choanal stenosis with stenting and acquired bilateral choanal stenosis without stenting, which are the different scenarios that may occur in CA/CS. Their management by surgical resection has been described and a review of the literature is done. The endoscopic choanoplasty surgery with resection of the posterior septal plate and medial part of the pterygoid has a good success rate in all the three scenarios.
End Note
Author Information
- Dr. Sajith Babu Thavarool, MS, DNB; Senior Consultant and Head of Department, Department of Head and Neck Surgery, Aster MIMS, North Kerala Cluster
- Dr. Manu Santosh, MS, Specialist, Department of Head and Neck Surgery, Aster MIMS, Kannur
- Dr. Ram Guruprasad, Fellow, Department of Head and Neck Surgery, Aster MIMS, Calicut
- Dr. Janani Anandkumar, Fellow, Department of Head and Neck Surgery, Aster MIMS, North Kerala Cluster
- Dr. Mihir Mohan, Senior Specialist, Department of Head and Neck Surgery, Aster MIMS, North Kerala Cluster
Confliction of Interest: We, the authors have no conflict of interest to disclose regarding this manuscript
References
- Otto AW. XXIII. Lehrbuch der Pathologischen Anatomie des Menschen und der Thiere. Am J Med Sci. 1831;1(15).
- Zaidi A, Dey AC, Sabra O, James J. Bilateral congenital choanal atresia in a preterm neonate - a rare neonatal emergency: A case report and review of literature. Med J Armed Forces India. 2024;80(1).
[Pubmed] | [Crossref] - Benjamin RH, Marengo LK, Scheuerle AE, Agopian AJ, Mitchell LE. Prevalence and descriptive epidemiology of choanal atresia and stenosis in Texas, 1999–2018. Am J Med Genet A. 2024.
[Pubmed] | [Crossref] - Kwong KM. Current Updates on Choanal Atresia. Vol. 3, Frontiers in Pediatrics. 2015.
[Pubmed] | [Crossref] - Sgayer I, Lowenstein L, Odeh M. Antenatal ultrasound findings in choanal atresia: A case report and review of the literature. Case Rep Womens Health. 2024;41.
[Pubmed] | [Crossref] - Urbančič J, Vozel D, Battelino S, Boršoš I, Bregant L, Glavan M, et al. Management of Choanal Atresia: National Recommendations with a Comprehensive Literature Review. Children. 2023;10(1).
[Pubmed] | [Crossref] - Poch VIÑALS R, Calvo RR. Choanal Atresia: An Embryological, Clinical, and Therapeutical Study. AMA Arch Otolaryngol. 1956;63(6).
[Pubmed] | [Crossref] - Petkovska L, Petkovska I, Ramadan S, Aslam MO. CT evaluation of congenital choanal atresia: Our experience and review of the literature. Australas Radiol. 2007;51(3).
[Pubmed] | [Crossref] - Vanzieleghem BD, Lemmerling MM, Vermeersch HF, Govaert P, Dhooge I, Meire F, et al. Imaging studies in the diagnostic workup of neonatal nasal Obstruction. J Comput Assist Tomogr. 2001;25(4).
[Crossref] - Hengerer AS, Strome M. Choanal atresia: A new embryologic theory and its influence on surgical management. Laryngoscope. 1982;92(8).
[Pubmed] - Blake KD, Davenport SLH, Hall BD, Hefner MA, Pagon RA, Williams MS, et al. Charge association: An update and review for the primary pediatrician. Vol. 37, Clinical Pediatrics. 1998.
[Pubmed] | [Crossref] - Carl Emmert. Lehrbuch der Chirurgie: Lehrbuch der speciellen Chirurgie. . Vol. Volume 2. Sturtgurt: Berlag Von Rub Dann; 1854.
- Hengerer AS, Brickman TM, Jeyakumar A. Choanal atresia: Embryologic analysis and evolution of treatment, a 30-year experience. Vol. 118, Laryngoscope. 2008 May;118(5):862-6.
[Pubmed] | [Crossref] - Durmaz A, Tosun F, Yldrm N, Sahan M, Kvrakdal C, Gerek M. Transnasal endoscopic repair of choanal atresia: results of 13 cases and meta-analysis. J Craniofac Surg. 2008 Sep;19(5):1270–4.
[Pubmed] | [Crossref] - Bartel R, Levorato M, Adroher M, Cardelus S, Diaz A, Lacima J, et al. Performance of endoscopic repair with endonasal flaps for congenital choanal atresia. A systematic review. Vol. 72, Acta Otorrinolaringologica Espanola. 2021 Jan-Feb;72(1):51-56.
[Pubmed] | [Crossref] - Sinha V, Talagauara Umesh S, Jha SG, Dadhich S. Choanal Atresia: Birth Without Breath. Indian Journal of Otolaryngology and Head and Neck Surgery. 2018;70(1).
[Pubmed] | [Crossref] - Wilcox LJ, Smith MM, de Alarcon A, Epperson M, Born H, Hart CK. Use of Steroid-Eluting Stents after Endoscopic Repair of Choanal Atresia: A Case Series with Review. Annals of Otology, Rhinology and Laryngology. 2020;129(10).
[Pubmed] | [Crossref] - Tomoum MO, Askar MH, Mandour MF, Amer MA, Saafan ME. Stentless mirrored L-shaped septonasal flap versus stented flapless technique for endoscopic endonasal repair of bilateral congenital choanal atresia: A prospective randomised controlled study. Journal of Laryngology and Otology. 2018;132(4).
[Crossref]