Original Research Published on June 20, 2024
A Prospective Study of Clinical Profile of
Primary Otomycosis
Vidya P V1, Ravi A1, Mary Abraham1, Mihir Mohan T1, Sajith Babu1
1. Department of Otorhinolaryngology, MIMS Calicut, Kerala*
ABSTRACT
Introduction: Otomycosis, a common otological problem is difficult to manage and necessitates patient compliance due to a high recurrence rate.
Materials and Methods: A prospective comparative study on clinical profile of primary otomycosis from January 2023 to October 2023. 152 immunocompetent individuals were studied. 76 patients with clinically diagnosed otomycosis included in the study group.76 patients without clinical otomycosis or any other aural symptoms seeking treatment for non otological problems were included in the control group. The objective was to know the clinical profile of primary otomycosis and identification of predisposing factors.
Results: Otomycosis is predominantly a unilateral disease and more common in lower socioeconomic status. Commonest symptom was ear itching. Individuals who habitually engage in self-cleaning practices and use home remedies for ear relief are at an elevated risk of otomycosis.
Conclusion: Patient education, aural hygiene and topical antifungal treatment aid in control of progression of this disease.
Keywords: Otomycosis, Ear Diseases, Fungal Infection, Aspergillus
INTRODUCTION
Otomycosis is a fungal infection that affects the skin of the external ear canal. It is frequently encountered in a general otolaryngology clinic, with reported prevalence rates ranging from 9% to 27.2 % among patients exhibiting signs and symptoms of otitis externa.1 This condition is found across the globe but exhibits a higher incidence in regions characterized by hot, humid and dusty climates particularly in tropical and subtropical areas. Fungi can either be the primary causative agent or can occur in conjunction with bacterial infections. Several factors have been proposed as potential predisposing factors to otomycosis such as humid climate, ear instrumentation, immunocompromised conditions, growing utilization of antibiotics drops and steroid preparations.
In the early stages of otomycosis, patient often report severe itching, which can progress to pain, hearing loss and in some cases lead to tympanic membrane perforation. While Aspergillus niger and Candida albicans are the most frequently implicated culprits, its worth noting that otomycosis can be caused by a diverse array of other fungal species as well. The diagnosis primarily relies on clinical assessment and further confirmation obtained through fungal smear and culture tests
Otomycosis can be categorized as primary or secondary. Primary otomycosis is diagnosed when otomycosis is present in the EAC of an immunocompetent individual and in the presence of an intact tympanic membrane and absence of any other external or middle ear pathology. Secondary otomycosis is diagnosed when otomycosis present in the EAC or middle ear of patients with history of major trauma, surgery or fungal infections in other parts of the body. It can occur in immunocompetent persons and in those with immunocompromised conditions like HIV, diabetes mellitus, or granulomatous diseases or other immunocompromised conditions detected by lab studies.
Managing the disease can be daunting and frustrating experience for both patients and otolaryngologists. It often demands a good compliance and regular follow up because of high chance of recurrence.2 Mainstay of treatment involves removal of debris, thorough toileting of the external ear and the use of topical antimycotic agents such as clotrimazole. Systemic agents are warranted only in the severe forms of the disease.
This study conducted at a tertiary care hospital in North Kerala, is dedicated to investigate the clinical profile and factors predisposing to primary otomycosis
MATERIALS AND METHODS
The study was conducted among patients with primary otomycosis at the Department of ENT, MALABAR INSTITUTE OF MEDICAL SCIENCES, Calicut, Kerala. It is a prospective comparative study from January 2023 to October 2023. A total of 152 immunocompetent individuals attending the outpatient department were chosen for the study.76 patients with clinically diagnosed otomycosis in the absence of other ear conditions were considered as primary otomycosis and was included in the study group. 76 patients without clinical otomycosis or any other aural symptoms seeking treatment for non otological problems were included in the control group.
The criteria used for establishing a diagnosis of otomycosis were presence of the following findings:
- presence of symptoms like itching, pain, feeling of blocked ear, tinnitus, deafness, and otoscopy revealing masses of hyphae/spores or a curd-like grey/white discharge
- the demonstration of fungal elements in 10% potassium hydroxide-methylene blue preparation
The following conditions were classified as secondary otomycosis and was excluded from the study:
- all patients with otomycosis alongside history of chronic otitis media, active otitis, tympanic membrane perforations, prior ear surgery or aural procedures, and diabetics,
- patients with any serious debilitating diseases like malignancies, tuberculosis, and other chronic granulomatous diseases,
- patients with immunocompromised conditions and history suggestive of fungal diseases elsewhere in the body
DATA COLLECTION METHOD
After obtaining consent from all patients involved in the study, demographic data, clinical features and predisposing factors are noted in both study and control group. KOH staining and routine culture done in the study group. Patients treated according to standard treatment protocol. Collected data were recorded using data collection proforma.
METHODOLOGY
Scientific Committee and Institutional Ethical Committee clearance were obtained prior to the study. Informed and written consent were taken from all patients involved in the study. The demographic data of the patient including age, sex, socioeconomic status, and occupation were recorded. Clinical presentations of cases recorded. History of use of wooden sticks, metal objects or any other materials for wax removal, history of swimming, use of oils, over the counter use of topical antibiotic ear drops or other ear preparations elicited in both study and control group. Otoscopic examination done. External ear canal, skin and status of tympanic membrane assessed. Presence of masses of hyphae or spores or a curd like grey or white discharge noted.
SAMPLE COLLECTION AND PROCESSING
EAC of each patient was meticulously examined for signs of fungal infection related debris. Using sterile swabs samples were collected from the EAC and promptly transported to the laboratory within thirty minutes for both mycological and bacteriological evaluation .All samples underwent assessment through both direct examination and culture methods. For mycological identification, a direct microscopic examination was conducted using a 10 % KOH examination method. For bacterial assessment, a portion of the sample was cultured on blood and MacConkey agar at 37 degree Celsius for 48 hours to detect bacterial growth. Identification of bacterial isolates was carried out using standard bacteriological procedures. Most fungi grow in current bacteriological media and such growth observed were documented.
Following sample collection all patients were subjected to thorough aural toilet and treated according to standard treatment protocol. Data obtained will be analysed with a statistical software program.
STATISTICAL METHODS
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 26.0) and graphs were depicted using Microsoft excel or open office Spreadsheet. Normality of distribution of all data were assessed using histograms and Kolmogorov–Smirnov/Shapiro-wilk test. Univariate analyses of characteristics were performed using independent sample test for normally distributed continuous variables and a Chi-square test for dichotomous variables. In case of a non-normal distribution, a Mann– Whitney test was used to compare groups. For all test a p value <0.05 was considered as statistically significant.
RESULTS
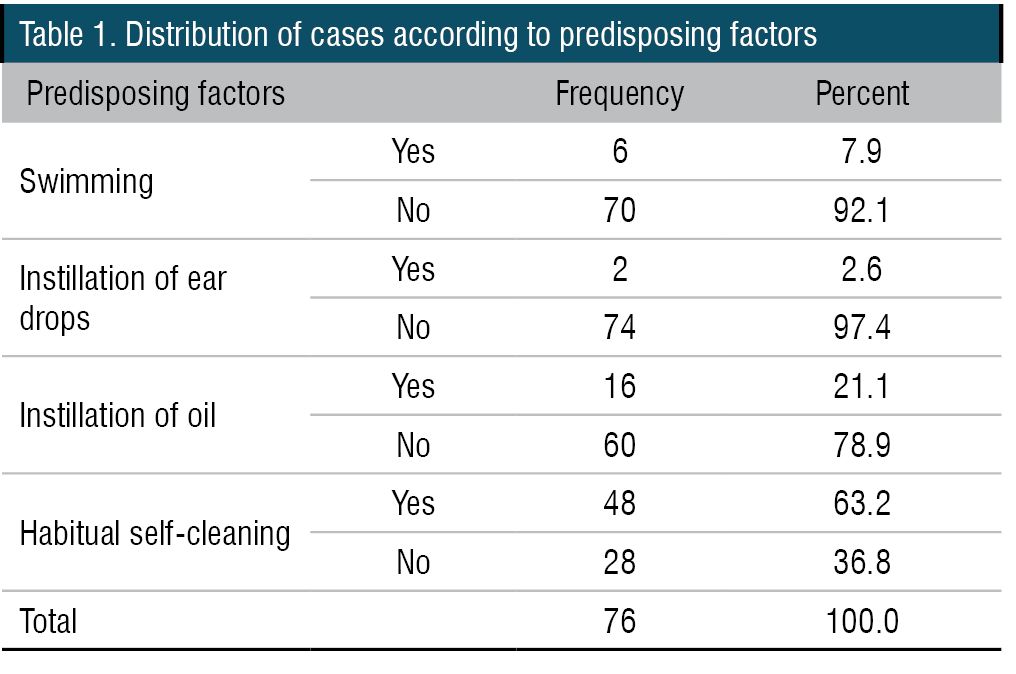
A total of 76 cases were enrolled. Age of cases ranged from 8 to 75 with a mean age of 41.3 (SD=18.37) years. 64.5% of the cases were females. 53.9% had had education up to high school. About three-fourths belonged to lower socioeconomic class.55.3% of the cases were unemployed. Majority of the cases were reported in June and July. Among the cases, all except one had ear itching. Ear block was the next most common symptom with 96.1% patients, followed by ear pain in 88.2%. Nearly three-fourths (73.7%) had ear discharge, while five patients had tinnitus. Majority (88.2%) had symptoms for less than a week. Three fourths of the patients had symptoms in the Right ear. Six cases mentioned they go swimming, two gave history of instilling of ear drops while 16 (21.1%) gave a history of instilling oil in ears. Habitual self-cleaning was common, with nearly two-thirds (63.2%) of cases stating that they habitually cleaned their ears. There were 22 (28.9%) with none of the above four predisposing factors (Table 1)
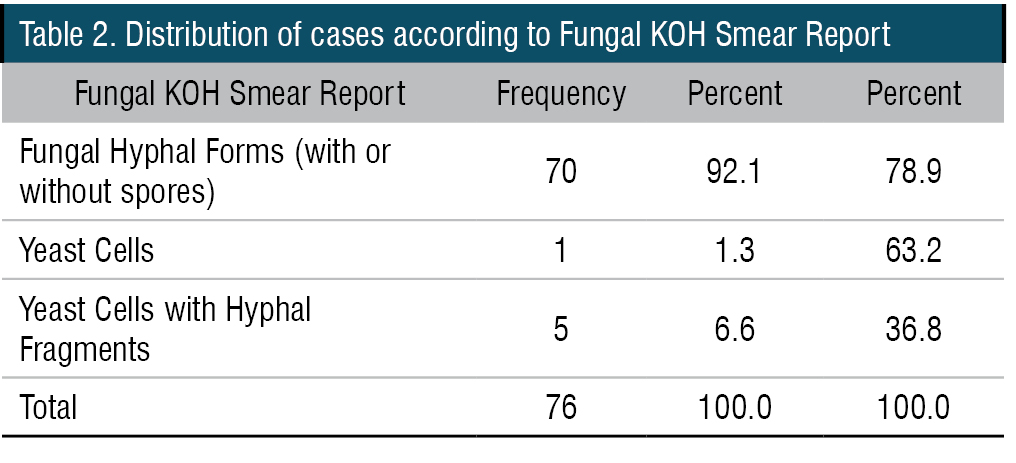
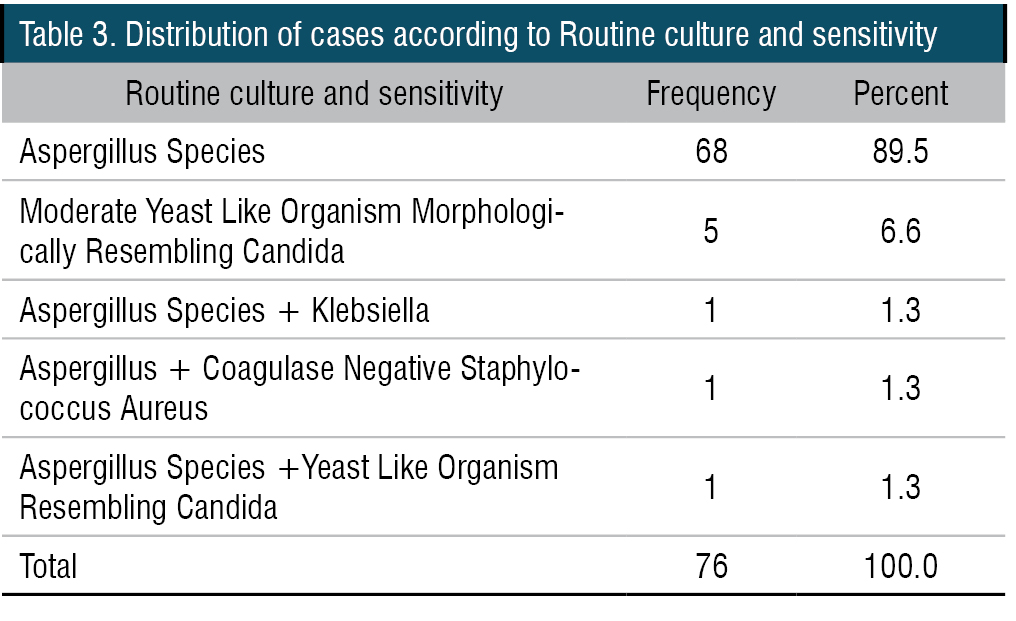
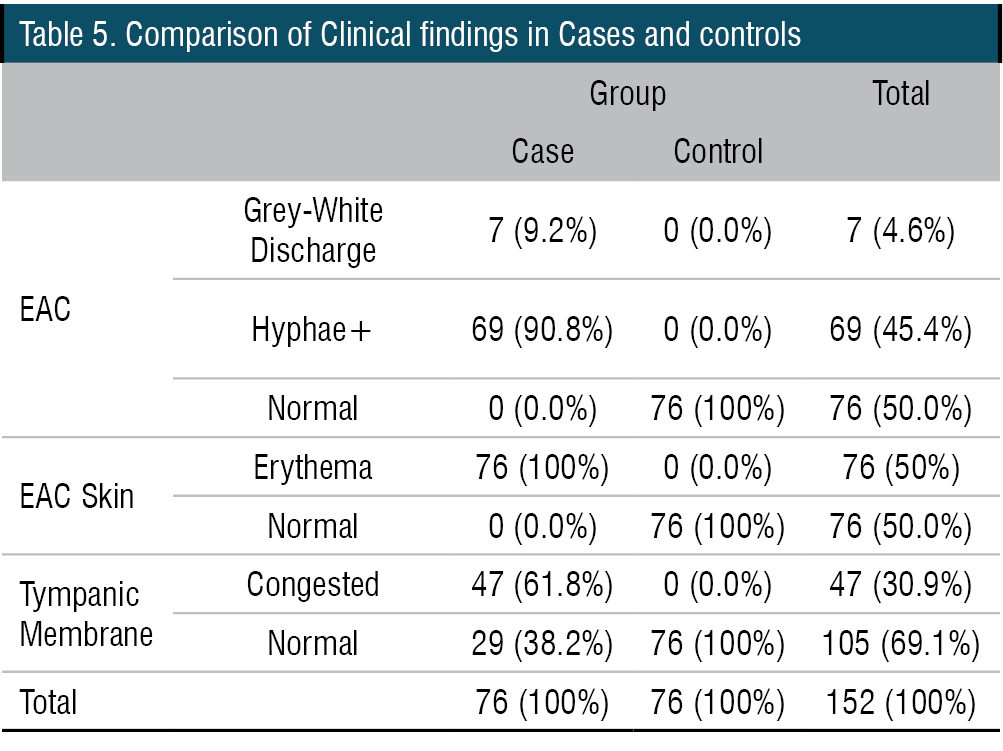
On examination of EAC, none appeared normal. 90.8% had hyphae. EAC Skin appeared erythematous in all cases 61.8 % had a congested tympanic membrane, while it was normal in 38.2%. Fungal KOH smear showed fungal hyphal forms in 92.1% cases; Yeast cells alone in one case and Yeast cells with hyphal fragments in five (6.6%) cases (Table 2). All cases had fungal growth on routine culture. Seventy cases (93.4%) had Aspergillus growth, with or without other growths. Mixed fungal and bacterial growth was observed in 2.6% of cases (Table 3). All except two (97.4%) had clinical improvement on their first follow-up. These two cases had clinical improvement on second follow-up. There was no significant difference in the age and sex distribution in cases and controls. The mean age in two groups were not significantly different. (p=0.623). There was a significant difference in the education status in cases and controls. Though there was no specific trend, proportion of those educated only up to high school was higher among cases. There was a significant difference in the Socioeconomic status of the cases and controls. Cases tend to be of Upper lower class while the controls were mostly of lower middle class. There was no significant difference in unemployment among the two groups.
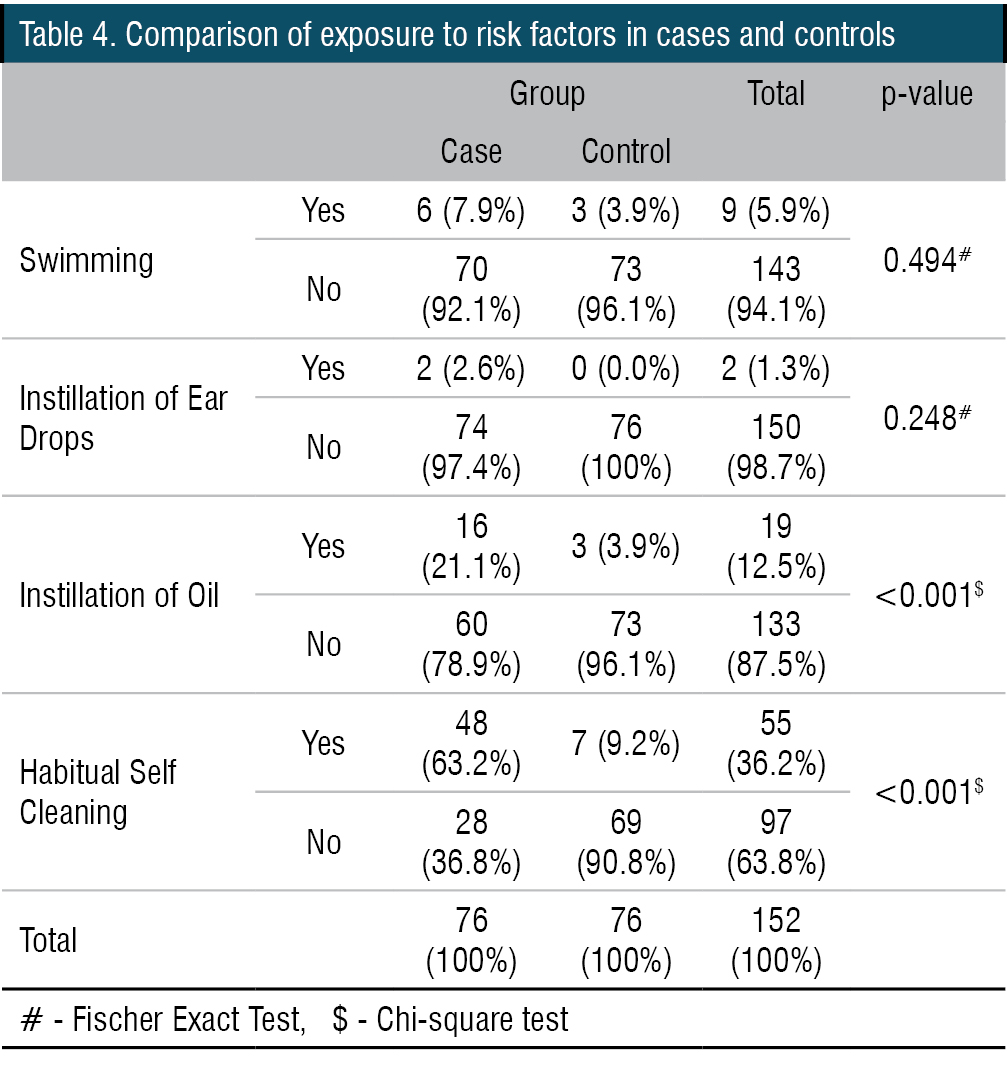
Swimming was not found to be associated with Otomycosis. [7.9% v/s 3.9%, p=0.494 – Fisher Exact]. Only two cases gave history of ear drop instillation, while there were none in control group. (0.248). Instillation of oil in ear was found to be significantly associated with otomycosis. [21.1% v/s 3.9%, p<0.001]. Similarly, habitual ear cleaning was also significantly associated with otomycosis. [63.2% v/s 9.2%, p<0.001]. EAC was normal in all controls while there where hyphae or discharge present in all cases (Table 4). Similarly, cases had congested or erythematous EAC skin while all controls had normal EAC skin. Tympanic membrane was normal on 38.2% of the cases while all controls had normal TM (Table 5). Statistical significance cannot be commented upon in any of these comparisons.
DISCUSSION
Otomycosis, a fungal infection affecting the external auditory canal, is widespread, with a higher prevalence in hot, humid, and dusty regions of the tropics and sub-tropics. Various factors, including humid climates, ear instrumentation, immunocompromised states, increased use of antibiotic drops, and steroid preparations, have been suggested as potential contributors to otomycosis. Patients frequently complain of intense itching, which may escalate to pain, hearing impairment, and, in severe cases, even tympanic membrane perforation. Diagnosis is established through clinical assessment, complemented by fungal smear and culture tests. Aspergillus niger and Candida albicans are commonly implicated offenders
Otomycosis can be classified as primary or secondary. Primary otomycosis is identified when an immunocompetent individual exhibits otomycosis in the external auditory canal, with an intact tympanic membrane and no other ear pathology. On the other hand, secondary otomycosis is diagnosed when the infection is present in individuals with a history of trauma, surgery, or fungal infections elsewhere in the body. It can manifest in both immunocompetent and immunocompromised individuals, the latter including conditions such as HIV, diabetes mellitus, or granulomatous diseases.
Effectively managing otomycosis proves to be a challenging and sometimes exasperating experience for both patients and otolaryngologists. Successful treatment often hinges on patient compliance and regular follow-ups, given the high likelihood of recurrence.
Sociodemographic details
A total of 76 cases were studied. Age of cases ranged from 8 to 75 with a mean age of 41.3 (SD=18.37) years. The highest number of cases belonged to (15-29) and (45-59) age group. The lowest incidence was in the < 15 years age group. This was in accordance with the study conducted by Yehia et al in which similar distribution of cases with respect to age was observed.3 Studies conducted by vishwanatha et al and Bibhu Pradhan et al states that more number of cases were in the age group of 21-30 years.4,5
49 out of 76 cases were females and 26 were males. i.e. 64.5% of the cases were females. This is in accordance with study conducted by Yehia et al in which 65.4 % cases were females. This is in contrast to a study conducted by Sampath Chandra Prasad et al, Yassin et al and Ravinder kaur.1,6,7 Aneja et al. attribute the heightened incidence of otomycosis in females to the wearing of traditional head coverings, such as veils or purdah.8 This practice may elevate humidity within the ear canal, creating an optimal environment for fungal growth and predisposing individuals to otomycosis. Additionally, the use of a hair dryer in the context of wet hair among women is another factor that could contribute to increased humidity in the external ear canal, fostering an ideal environment for fungal growth and promoting otomycosis.9
Only up to the high school level was the extent of education for 53.9% cases. There was a significant difference in the education status in cases and controls. Though there was no specific trend, proportion of those educated only up to high school was higher among cases.
55.3% of the cases were unemployed among cases. There was no significant difference in unemployment among the two groups
A marked difference in socioeconomic status was evident between the cases and controls. Cases tended to belong to the upper-lower class, whereas the controls were predominantly from the lower-middle class. This was in agreement with previous reports that stated an increased incidence in people of lower socioeconomic status
Clinical presentation of cases
Majority of the cases reported in the month of June and July. This correlates with the study of Than K M. et al who found increased incidence of Otomycosis during the rainy seasons.9 Agrawal et al also stated that high humidity during the monsoon months favoured the development of Otomycosis.10
In our study the commonest symptom was ear itching 75 (98.7%) followed by ear block73 (96.1%), ear pain 67 (88.2%). Nearly three-fourths 56 (73.7%) had ear discharge, while five (6.6%) patients had tinnitus. Paulose et al found that itching was the most common symptom (88%) followed by ear block (87.5%), discharge (30%) and tinnitus (22%).11 Oliveri S et al also found itching as the characteristic symptom of Otomycosis followed by pain and loss of hearing.12 In contrast Ravinder et al found ear block as the commonest symptom (93.7%) followed by itching (71.5%).7 Majority (88.2%) had symptoms for less than a week.
All 76 cases, as indicated by various studies, consistently showed the disease to be unilateral. This observation lends support to the notion that the disease is not highly infectious.10,16 Moreover, symptoms were predominant in the right ear for three-fourths of the patients.
Predisposing factors
Out of the 76 cases, six individuals reported engaging in swimming activities and it was not found to be associated with Otomycosis. [p=0.494]. Contrary to this, findings reported by Aneja et al. and Paulose et al. indicate a correlation between otomycosis and swimming.
Two cases disclosed a history of ear drop usage, while there were none in control group. (p=0.248). This aligns with the study conducted by Tang Ho et al., where no such association was identified. However, in a study by Sampath Chandra Prasad et al., the use of topical antibiotic ear drops was observed in 20% of cases. 16 (21.1%) mentioned instilling coconut oil in their ears and it was found to be significantly associated with otomycosis. [21.1% v/s 3.9%, p<0.001]. This aligns with the study conducted by Priyanka Debta et al., attributing it to the sporostatic nature of coconut oil.13 This property aids in preserving the viability of conidia in the external auditory canal for an extended period, facilitating the development of otomycosis.
Habitual self-cleaning was more common, with approximately two-thirds (63.2%) of cases indicating a regular practice of cleaning their ears and it had a significant association with otomycosis. [63.2% v/s 9.2%, p<0.001]. This aligns with the findings observed in the study conducted by Agarwal et al . Ear cleaning habits might play a role in pathogenesis, as traumatized skin in the external ear canal could provide a favourable condition for fungal growth.10 Notably, 22 cases (28.9%) did not exhibit any of the predisposing factors observed in the remaining cases.
Clinical Findings
On examination of EAC, none appeared normal. 90.8% had hyphae. 9.2 % had grey white discharge in EAC. EAC Skin appeared erythematous in all cases. 61.8 % had a congested tympanic membrane, while it was normal in 38.2%. These findings correlate with those observed by Paulose et al. and Mugliston et al.11,14
Fungal KOH smear report
Fungal KOH smear showed fungal hyphal forms alone in 92.1% cases; Yeast cells alone in one case and Yeast cells with hyphal fragments in five (6.6%) cases.
Routine culture and sensitivity report
All cases had fungal growth on routine culture. Seventy cases (93.4%) had Aspergillus growth, with or without other growths. Yeast Like Organism Morphologically Resembling Candida were observed in 5 (6.6%) cases. Literature review reveals that the predominant organisms isolated in otomycosis are of the Aspergillus species, followed closely by Candida.1
Two (2.6 %) cases had mixed fungal and bacterial growth and the bacteria cultured were Klebsiella and coagulase negative Staphylococcus aureus. This is similar to findings observed by Ravinder Kaur et al in which there were 2.8 % mixed infections. Staphylococcus aureus, P. aeruginosa, and Proteus spp. were dominant bacterial pathogens reported in other studies.1
Treatment
Though there are no consensus on the most effective agent in otomycosis, azole family are the ones that are commonly used. These synthetic agents work by decreasing the concentration of ergosterol, a crucial sterol in the normal cytoplasmic membrane. Among the topical azoles, clotrimazole takes the lead in popularity. Its effectiveness in managing otomycosis is noteworthy, boasting a reported success rate ranging from 95% to 100%. Notably, clotrimazole goes beyond its antifungal role—it also exhibits antibacterial effects. This dual action makes it particularly advantageous when tackling infections that involve a mix of bacteria and fungi.15
Topical clotrimazole has been used to treat all cases after thorough suction clearance of EAC to remove all visible fungal debris. A combination of clotrimazole cream, antibiotic neomycin and a steroid is drawn into syringe and is carefully applied to the ear canal using a suction tip and a follow-up is conducted one week later.
Clinical Improvement over Follow-up
All except two (97.4%) had clinical improvement on their first follow-up. These two cases had clinical improvement on second follow-up. This is in accordance with the study conducted by Tang Ho et al., in which more than 80% of cases showed improvement within 2 weeks.
CONCLUSION
All the primary otomycosis cases manifested as unilateral disease and right ear was involved in three fourths of the patients. There was no age-wise or sex wise variation in the occurrence of primary otomycosis. Majority of patients belonged to lower socioeconomic status. Most of the cases reported in the month of June and July. Ear itching and ear block were the commonest symptoms. More than 80 % presented with less than a week duration of symptoms. Habitual self cleaning is the commonest predisposing factor of primary otomycosis followed by coconut oil application. None of the ear canal appeared normal. It contained either hyphal mass or discharge. Tympanic membrane appeared congested in majority of cases. The KOH smear revealed a fungal hyphal mass in the majority of cases. Routine culture and sensitivity revealed Aspergillus in more than 90% of cases. Following thorough aural toilet and topical antifungal application, clinical improvement was achieved in more than 95 % cases on first follow up.
End Note
Author Information
- Dr. Vidya P.V, DLO, DNB ENT, Department of Otorhinolaryngology, MIMS Calicut, Kerala
- Dr. Ravi A, MS ENT, Department of Otorhinolaryngology, MIMS Calicut
- Dr. Mary Abraham, DLO, MS ENT, Department of Otorhinolaryngology, MIMS Calicut, Kerala
- Dr. Mihir Mohan T., DNB (ENT), MNAMS, FHNS, Department of Otorhinolaryngology, MIMS Calicut, Kerala
- Dr Sajith Babu TP, MS, DNB ENT, FHNS, GOLF, Department of Otorhinolaryngology, MIMS Calicut, Kerala
Financial support: Nil
Confilict of Interest: None declared
REFERENCES
- Prasad SC, Kotigadde S, Shekhar M, Thada ND, Prabhu P, D’ Souza T, Prasad KC. Primary otomycosis in the Indian subcontinent: Predisposing factors, microbiology, and classification. Int J Microbiol. 2014;2014:636493.
[Pubmed] | [Crossref] - Kumar, “Fungal spectrum in otomycosis patients,” JK Science, vol. 7, no. 3, pp. 152–155, 2005. (n.d.).
[Source] - Yehia MM, al-Habib HM, Shehab NM. Otomycosis: A common problem in north Iraq. J Laryngol Otol. 1990 May;104(5):387-9.
[Pubmed] | [Crossref] - Viswanatha B, Sumatha D, Vijayashree MS. Otomycosis in immunocompetent and immunocompromised patients: Comparative study and literature review. Ear Nose Throat J. 2012 Mar;91(3):114-21.
[Pubmed] | [Crossref] - Pradhan B, Tuladhar NR, Amatya RM. Prevalence of otomycosis in outpatient department of otolaryngology in Tribhuvan University Teaching Hospital, Kathmandu, Nepal. Ann Otol Rhinol Laryngol. 2003 Apr;112(4):384-7.
[Pubmed] | [Crossref] - Yassin A, Maher A, Moawad MK. Otomycosis: A survey in the eastern province of Saudi Arabia. J Laryngol Otol. 1978 Oct;92(10):869-76.
[Pubmed] | [Crossref] - Kaur R, Mittal N, Kakkar M, Aggarwal AK, Mathur MD. Otomycosis: A clinicomycologic study. Ear Nose Throat J. 2000 Aug;79(8):606-9.
[Pubmed] - Aneja KR, Sharma C, Joshi R. Fungal infection of the ear: A common problem in the north eastern part of Haryana. Int J Pediatr Otorhinolaryngol. 2010 Jun;74(6):604-7.
[Pubmed] [Crossref] - Than KM, Naing KS, Min M. Otomycosis in Burma, and its treatment. Am J Trop Med Hyg. 1980 Jul;29(4):620-3.
[Pubmed] | [Crossref] - Agarwal P, Devi LS. Otomycosis in a Rural Community Attending a Tertiary Care Hospital: Assessment of Risk Factors and Identification of Fungal and Bacterial Agents. J Clin Diagn Res. 2017 Jun;11(6):DC14-DC18.
[Pubmed] | [Crossref] - Paulose, K., Khalifa, S., Shenoy, P., & Sharma, R. (1989). Mycotic infection of the ear (otomycosis): A prospective study. The Journal of Laryngology & Otology, 103(1), 30-35.
[Pubmed] | [Crossref] - Oliveri S, Capello G, Napolitano MG, Triolo C, Grillo C. [Otomycosis: etiology and analysis of predisposing factors]. Boll Ist Sieroter Milan. 1984;63(6):537–42.
[Pubmed] - Debta P, Swain SK, Lenka S, Sahu MC. Otomycosis: A Comprehensive Review. Indian Journal of Forensic Medicine & Toxicology. 2020 Oct 29;14(4):8429–32.
[Crossref] - Mugliston, T., & O’Donoghue, G. (1985). Otomycosis—A continuing problem. The Journal of Laryngology & Otology, 99(4), 327-333.
[Pubmed] | [Crossref] - Ho T, Vrabec JT, Yoo D, Coker NJ. Otomycosis: Clinical features and treatment implications. Otolaryngol Head Neck Surg. 2006 Nov;135(5):787-91.
[Pubmed] | [Crossref]