Original Research Published on December 30, 2022
Clinical Analysis of Techniques and Complications in 414 Consecutive Cochlear Implantations
Kavitha Gauthaman1, Manoj Manikoth1
1. Dr. Manoj’s ENT Super Specialty Institute & Research Centre, ( MESIARC), Kozhikode*
ABSTRACT
Aim: To report the frequency of surgical complications following 414 consecutive cochlear implant surgeries (402 children; 12 adults), of whom 323 underwent standard incision and 91 minimal access incision and to analyze the feasibility of using the minimal access approach in all CI candidates. A careful assessment was performed to analyze whether the latter approach is more advantageous than the former in different quality parameters.
Methods: Retrospective analysis of patients who underwent cochlear implant surgery from February 2012 to February 2019 by the same surgeon at a single center.
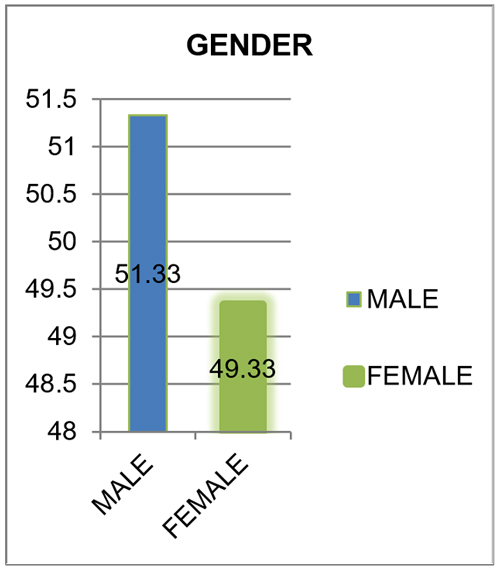
Patients: 414 consecutively implanted patients (male: 51.33% female: 49.33%, Right: 68.66% Left: 26.66%, Bilateral: 4.66%).323 underwent a standard incision (Lazy S) and 91 underwent a minimal access incision. The average age of the standard incision group was 4.3years (range 9months-73years); that of the minimal access group 8.6 years (Range 9months-64years). The average incision size in the standard incision group was 7.61 cm and that of the minimum access group was 4.53cm.
Results: Of the 414 patients who underwent surgery there were 30 surgery related complications (12 major, 18 minor), 11 device related complications. Major complications (5.3%) included wound infection (3); device extrusion (1); electrode displacement (2); temporary CSF leak (5) (in patients with cochleovestibular dysplasia’s); magnet displacement (1). The minor complications included transient facial paresis (3); vertigo (2); seroma (9); hematoma (1); tinnitus (3). There were 11 device failures, one secondary to trauma the overall complication rate (9.6%) was low in our center when compared against available literature
The mean operative time was 76 minutes for standard incision and 79.5minutes for the minimal access approach. A counter sink well for the receiver stimulator array was created and tie down of the device was done in all patients irrespective of the incision, except when a thin implant was used.
Clinical Significance: Cochlear implantation is a low-risk procedure when performed by an experienced surgeon following standard protocol. Detailed preoperative workup, study of access and tailoring of the approach to suit each patient is a necessity to prevent complications. The minimal access incision causes less morbidity, is cosmetically more acceptable to patients and offers sufficient access to perform a cochlear implantation without compromising on vital steps.
Introduction
Cochlear implantation is to this day the most effective treatment for severe to profound hearing loss.1-3 As of 2016 there were 600,000 cochlear implant recipients worldwide.
Devices and techniques are constantly evolving. It is a fairly low risk procedure in the hands of a trained and experienced surgeon. Although the incidence and severity of complications are comparatively low, identification and management of these complications are important and essential for a good implantation program.
The techniques of cochlear implantation are constantly evolving, with the lesser invasive minimal access techniques emerging as the preferred method for surgeons and patients. In this study we analyzed complications retrospectively, addressed their management and discussed the feasibility of using the minimal access technique for all patients.
Materials and methods
Patients
The study included 414 patients (430 cochlear implants). The cochlear implantations were performed serially by a single surgeon (M.M) at a single center from February 2012 to February 2019. Inorder to avoid bias only the surgeries done by a single senior surgeon were included. The study was approved by the ethics committee of our institution.
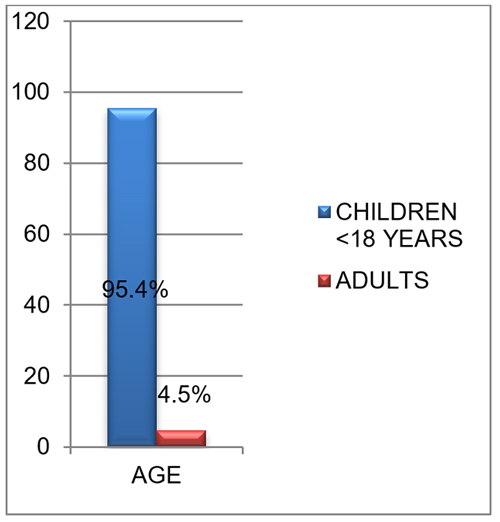
The series included 394(95.4%) unilateral and 20 bilateral (4.66%) implant recipients of which 212 were males (51.33%) and 202 were females (48.9%) [Figure 1], 95.4% were of children and less than 18 years of age and 4.5% were adults (Figure 2). 284(68.66%) underwent implantation in the right ear and 110(26.66%) in the left ear [Figure 3]
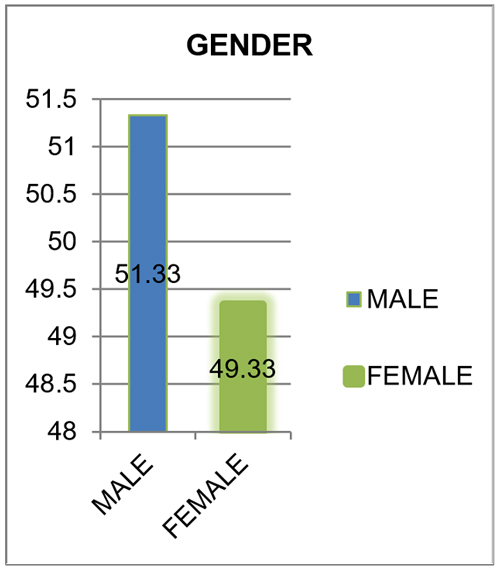
Figure 1. Gender distribution
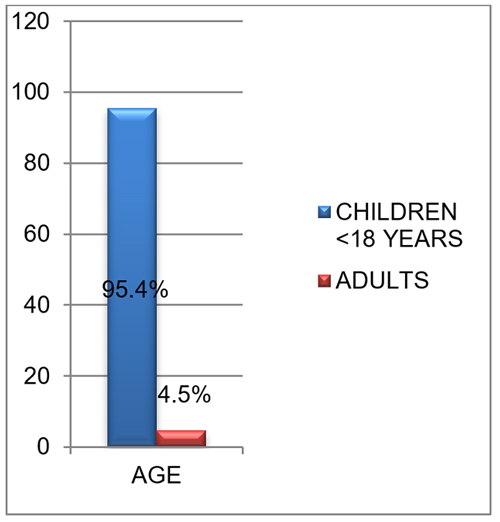
Figure 2. Age distribution

Figure 3. Side of implantation
Of the 414 patients 323 underwent a standard incision (LAZY S) and 91 underwent a minimal access incision. The average age at implantation for the standard incision group was 4.3years (range 9 months-73 years); that of the minimal access group 8.6 years (Range 9months-64years). The mean follow-up period was 6years (3years-9years).
There were 19 cases of inner ear malformations including 10 cases of vestibulocochlear anomalies – cases of Incomplete partition 2, Incomplete partition 3, and large vestibular aqueduct syndrome [Figure 4]
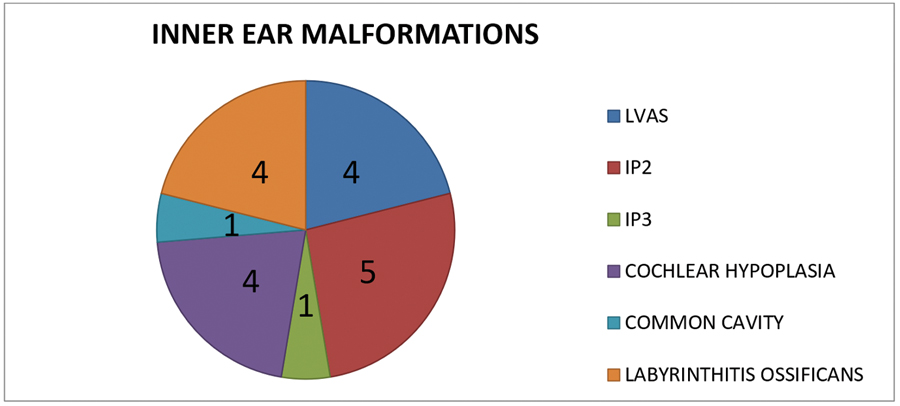
Figure 4. Distribution of inner ear malformation
In this study we did not attempt to compare the difference in the complication rates of the two different types of access as the patient numbers were insufficient to provide an unbiased result.
Revisions and re-implantations from other centers were not included in the study
Surgical Technique
Until 2018 both the standard incision and minimal access incision were used, with the minimal access incision being used more selectively in older children and adults. However, since 2018 the minimal access approach has been used exclusively.
STANDARD INCISION:
The standard (Lazy S) incision starts near the mastoid tip, curves 2cm behind the post aural groove and gets extended till the part where the pinna leaves the scalp and then takes a gentle 120 degree turn backwards and is about 6-8 cm long. The incision is deepened just below the post aural muscles and elevated anteriorly in a bloodless plane till the lower end of the temporal line, the sternocleidomastoid muscle attachment and the posterior canal wall edge is palpable. A posteriorly based periosteal flap is raised from just behind the posterior canal edge. The flap is elevated far backwards till the site of the receiver stimulator array is reached. This approach requires hair removal of about 4cm around the incision site [Figure 5,6]

Figure 5. Standard incision

Figure 6. Deepening of the incision
MINIMAL ACCESS INCISION:
The minimal access incision is marked by placing BTE metal template behind the ear, and the incision is made 1-2mm behind the template about 3-4cm long, the avascular plane as above is taken anteriorly. The temporal line and the sternocleidomastoid attachment are identified as before. The flap is taken posteriorly based as before, but with an anterior flap also that is taken midway between the incision and the line of the posterior canal wall. The anterior flap is raised till the external auditory canal margin is seen and then sutured anteriorly to the drapes. The posterior flap is elevated so that the RS package stays behind the incision. Shaving of hair is not required or minimal hair removal (0.5-1cm) is done in certain patients [Figure 7,8]

Figure 7. Minimal access incision

Figure 8. Posterior flap
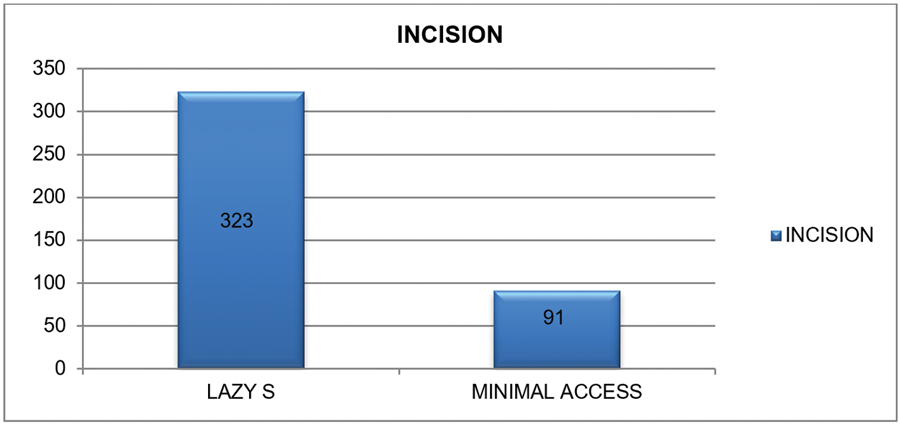
Figure 9. Distribution of incision
Cortical mastoidectomy is performed. The facial recess is identified and posterior tympanotomy done. The round window niche is identified. An O.6 mm diamond burr is then used to saucerise the area and expose the round window membrane. The Receiver / stimulator assembly is placed in the counter sink well and tied using ethibond excel polyester sutures. The round window membrane is opened with a pick leaving the spiral lamina undisturbed, and the basilar membrane is visualized. The electrode array is inserted through the round window and the reference electrode is pushed into the subperiosteal pocket below the temporalis muscle. The flap is closed over the stimulator and the wound is sutured in layers after perfect hemostasis. A pressure dressing is applied which is removed after 24 hours (Table 1).
Impedance telemetry is done after flap closure to check the impedance of all the electrodes. Electrically evoked compound action potentials are elicited.
Operative Protocol:
No preoperative antibiotics are given. Patients are advised shampooing and antibacterial ointment application in nose. A single dose of intravenous antibiotic is given 30 minutes prior to incision. Postoperatively oral antibiotics are given for 7 days.
Results
The overall incidence of complications was 9.6% (n=41). We divided these into surgery related complications (a)7.2% (n=30) and (b)device related complications (device failure) 2.6 %(n=11) [Figure 10]
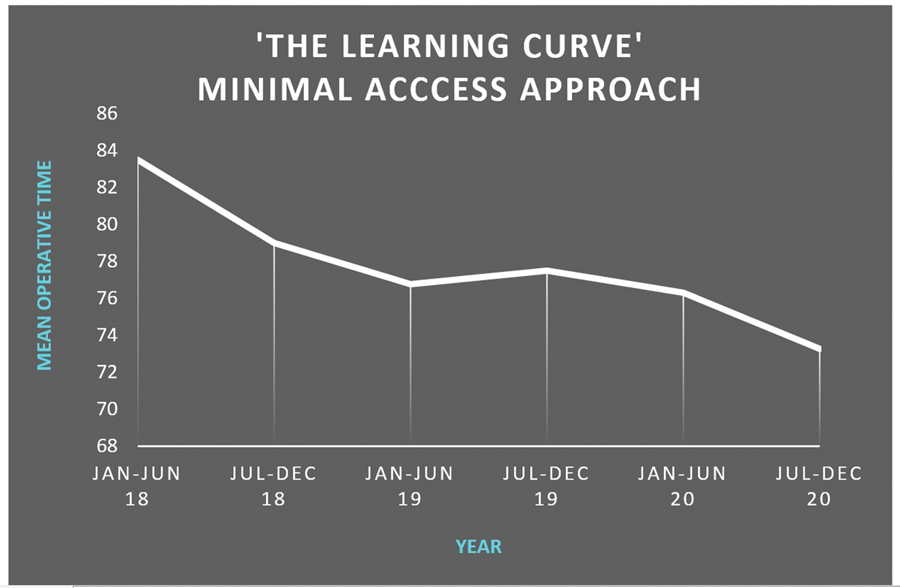
Figure 10. Learning curve - minimal access approach
The surgery related complications were classified as major and minor.
Major complications (5.3%) included wound infection (3); device extrusion (1); electrode displacement (2); temporary CSF leak (5) (in patients with cochleovestibular dysplasia); magnet displacement (1)
The minor complications (4.08%) included transient facial paresis (3); vertigo (2); seroma (9); hematoma (1); tinnitus (3).
There were 11 device failures, one secondary to trauma
The number of re-implantations were 17(4.1%) and the most common cause for reimplantation was hard device failure 70.6 % (n=12).
Major postoperative complications (Table 2)
Wound Infection:
Three cases of wound infection requiring reimplantation occurred (0.72 %).
In 2 patients wound infection occurred 3months after the initial implantation. Incision and drainage were done initially, but as there was no satisfactory healing.
Re-exploration was done, and the implant was found to be infected. The implant was removed leaving the electrode in situ and reimplantation was done after 3 months on the opposite side.
One patient presented as a delayed complication 5 years after the initial surgery. The patient developed discharge at the implant site. On exploration serous collection and possible biofilm formation was noted in the implant bed. The collection was cleared, and patient was started on oral antibiotic therapy. The patient was symptom free for 7 months. However, the discharge reoccurred and hence the device was explanted and reimplantation was done in the other ear.
Electrode Displacement:
Electrode displacement occurred in 2 cases (0.48%)
A post meningitic patient with labyrinthitis ossificans was implanted and during the initial surgery only partial insertion of the electrode into the basal turn had been possible. She developed purulent discharge from the implant site after 13 years.
On radiological examination: Only basal turn of cochlea was seen. Middle and apical turns were not seen, were completely ossified. The Electrode array tip was seen within the lateral aspect of basal turn.
She underwent explantation of the cochlear implant device. Three months later she was re-implanted in the same ear. Partial insertion was possible.
The other patient had undergone bilateral cochlear implantation. High impedance was observed in majority of the electrodes in the right ear during switch on. CT scan revealed shift in position of receiver stimulator assembly and migration of the electrode array from the cochlea.
On re-exploration the Receiver / stimulator assembly was found to be displaced upwards. The electrode array and reference electrode were found to be curled in the periosteal pocket. Reinsertion of the electrode could not be done since the electrode had lost its stiffness. Hence explantation and re-implantation was done.
Magnet displacement:
One patient (0.24%) developed this complication because of improper usage of a high-powered magnet. He presented with swelling over the implant site and on subsequent re-exploration the magnet was displaced and had to be re-implanted.
Device extrusion:
This was observed in one patient (0.24%). He developed swelling over the implant site on the 8th postoperative day, and was treated with antibiotics, however the symptoms persisted and on re-exploration the device was found to be extruded, was removed and reimplantation was done in the same ear after three months.
Per operative complications:
Temporary CSF leak:
This complication was seen in patients detected to have congenital inner ear malformations. In this series 21 patients having inner ear malformations received cochlear implants. Of these 5 patients (1.2%) experienced temporary CSF gushers. The CSF leak was controlled on table and sealed using periosteum, fat, and fibrin glue. No further medical intervention was done in the postoperative period.
Of the 5 patients, 2 were cases of Incomplete partition 2 (mondini), one was a patient with an enlarged vestibular aqueduct, another patient a case of cochlear dysplasia and the final one a case of cystic cochleovestibular malformation. The patients did not experience any symptoms in the postoperative period.
Minor complications: (Table 3)
Transient facial nerve paresis was observed in 3(0.7%) patients. No intraoperative exposure or abnormal location of the facial nerve was observed in these cases. However, exposure of the nerve to heat from the burr shaft during drilling has been thought to be a possible cause. The patients were treated with oral corticosteroids. Complete recovery was observed in 10-12 weeks.

2 patients (0.48%) complained of Vertigo after implantation. None of these were in the immediate postoperative period. On vestibular testing there was no nystagmus or any other vestibular signs. Patients were counseled and advised labyrinthine exercises.
Tinnitus was described by 3 patients (0.72%) post cochlear implantation
Seromas and collection not requiring re-implantation were observed in 9 patients (2.17%). this was managed conservatively with local drainage, rebandaging and antibiotics.
One patient presented with a hematoma (0.24%) which was aspirated.
These minor complications did not interfere with implant performance and no further problems have been observed in these patients till date.
Of the 11 device failures described 1 was secondary to trauma (patient fell and hit his head). 10(2.41%) were due to hard device failures.
There were no cases of primary electrode misplacement, cholesteatoma, meningitis, taste disturbance, persistent pain, or death due to implantation.
TYPES OF ACCESS:
The average age of the standard incision group was 4.3years (range 9months-73years); that of the minimal access group 8.6 years (Range 9months-64years). The average incision size in the standard incision group was 7.61 cm and that of the minimum access group was 4.53cm.
The mean operative time was 76 minutes for standard incision and 79.5minutes for the minimal access approach. A counter sink well for the receiver stimulator array was created and tie down of the device was done in all patients irrespective of the incision, except when a thin implant was used [Figure 9].
OPERATING TIME-THE LEARNING CURVE DEMONSTRATED:
While the mean operating time for the new minimal access incision was found to be 79.5 minutes, we found that this had decreased to 76.7 minutes during the second year and 74.2 minutes during the third year of practice thus demonstrating the learning curve experienced when attempting a new technique.
DISCUSSION
Evolution of incisions
The technique of cochlear implantation has constantly evolved over time with more importance being given to reduction in the complication rates and perceived radical nature of the surgery. Access and incisions have been constantly evolving with a shift toward minimal access approaches. The conventional incisions such as the ‘C’ and the ‘INVERTED U’, the ‘INVERTED J’, resulted in large flaps and were associated with complications such as flap necrosis, infection, and scalp numbness. Modifications such as the extended endaural incision were also found to be associated with increased risk of infection and scalp numbness.4 The long incisions also required a radical head shave and invariably a longer hospital stay which led to a perception amongst parents, children, and teachers that the child had undergone very major complicated surgery.5
Due to concerns with the problems associated with the standard long incisions, and this being the era of minimally invasive surgery, smaller incisions began to be evaluated. As early as 1995, Gibson et al4 described an almost straight incision placed in the postauricular crease. O’Donoghue6 described a postauricular incision barely longer than the width of the cochlear implant device. Several centers now use a minimal access incision which is an oblique postauricular incision of about 2-4cm.7
The advantages of using a minimal access incision are minimal hair shaving, less tissue elevation and manipulation, faster healing, lesser swelling, better cosmesis and the potential for earlier activation. The disadvantages are decreased visibility, need for more skin retraction and limited access for drilling the bony well for the receiver stimulator array. However, with the use of special retractors and instruments adequate exposure for drilling a well and tie down fixation has been possible even with the minimal access approach.
Complications of cochlear implant surgery
Cochlear implantation has gradually become a common surgical procedure and is being performed in numerous centers worldwide. However as with any surgical procedure it is associated with complications and as such there must be sufficient awareness about the incidence of these complications and how to manage them.
Several systems of classification of these complications have been proposed. Hansen et al proposed a consensus on CI complications which was widely accepted.8 We have classified the complications in our center based on this consensus.
The complications were classified as either Major or minor complications. The major complications were those which required either a further surgical procedure, prolonged treatment or were considered life threatening. Minor complications were those which did not require any further surgical procedure and those which could be treated on an outpatient basis. The major complications were further classified as either device related or surgical and surgical complications as either, early, or delayed (Table 2)
Using this system of classification, we found our overall complication rate to be 9.6% during a maximum follow-up period of 9 years which included device failures although many studies exclude device failures as a complication of the procedure. This was found to be well below the internationally reported rate of 16%.1
The complication rates currently reported in literature are 11.8% of minor complications and 3.2% of major complications.1,3,9,10 Our major complication rate of 2.6% (excluding device failures) and minor complication rate of 4.08% was found too similar and acceptable.
CONCLUSIONS
Cochlear implantation is a low-risk procedure when performed by an experienced surgeon following standard protocol. Detailed preoperative workup, study of access and tailoring of the approach to suit each patient is a necessity to prevent complications. This large volume center with low rate of complications shifted to a minimal access procedure for certain advantages, avoidance of hair removal, quicker healing time and faster surgery. However, no compromise was made with regards to safety and proper receiver stimulator or electrode placement. The study shows no increased incidence of complications in the minimal access arm of the study although the number of cases and follow-up period is not yet sufficient to justify these findings. Hence it is proposed that the minimal access surgical approach be used for all cases of cochlear implantation as it seems to achieve all the objectives of standard approach and seems to be associated with a lesser likelihood of complications while also being cosmetically more acceptable
End Note
Author Information
- Dr. Manoj M . P. , Head of Otoneurology and cochlear implant unit, Dr. Manoj’s ENT Super Specialty Institute & Research Centre, ( MESIARC), Kozhikode
- Dr. Kavitha Gauthaman Research Assistant, Dr. Manoj’s ENT Super Specialty Institute & Research Centre, ( MESIARC), Kozhikode
Conflict of Interest: None declared
REFERENCES
1. Venail F, Sicard M, Piron JP, et al. Reliability and complications of 500 consecutive cochlear implantations. Arch Otolaryngology Head Neck Surg 2008; 134:1276–81.
[Pubmed] | [Crossref]
2. Farinetti A, Ben Gharbia D, Mancini J, Roman S, Nicollas R, Triglia JM. Cochlear implant complications in 403 patients: comparative study of adults and children and review of the literature. Eur Ann Otorhinolaryngol Head Neck Dis. 2014 Jun;131(3):177–82.|
[Pubmed] | [Crossref]
3. Bhatia K, Gibbin KP, Nikolopoulos TP, O’Donoghue GM. Surgical complications and their management in a series of 300 consecutive pediatric cochlear implantations. Otol Neurotol. 2004 Sep;25(5):730–9.
[Pubmed] | [Crossref]
4. Gibson WP, Harrison HC, Prowse C. A new incision for placement of cochlear implants. J Laryngol Otol. 1995 Sep;109(9):821–5.
[Pubmed] | [Crossref]
5. James AL, Papsin BC. Device fixation and small incision access for pediatric cochlear implants. Int J Pediatr Otorhinolaryngol. 2004 Aug;68(8):1017–22.
[Pubmed] | [Crossref]
6. O’Donoghue GM, Nikolopoulos TP. Minimal access surgery for pediatric cochlear implantation. Otol Neurotol. 2002 Nov;23(6):891–4.
[Pubmed] | [Crossref]
7. Mangus B, Rivas A, Tsai BS, Haynes DS, Roland JT. Surgical techniques in cochlear implants. Otolaryngol Clin North Am. 2012 Feb;45(1):69–80.
[Pubmed] | [Crossref]
8. Hansen S, Anthonsen K, Stangerup SE, Jensen JH, Thomsen J, Cayé-Thomasen P. Unexpected findings and surgical complications in 505 consecutive cochlear implantations: a proposal for reporting consensus. Acta Otolaryngol. 2010 May;130(5):540–9.
[Pubmed] | [Crossref]
9. Balkany TJ, Hodges AV, Buchman CA, Luxford WM, Pillsbury CH, Roland PS, et al. Cochlear implant soft failures consensus development conference statement. Otol Neurotol. 2005 Jul;26(4):815–8.
[Pubmed] | [Crossref]
10. Cohen NL, Hoffman RA. Complications of Cochlear Implant Surgery in Adults and Children. Ann Otol Rhinol Laryngol. 1991 Sep 1;100(9):708–11.
[Crossref]
11. Gysin C, Papsin BC, Daya H, Nedzelski J. Surgical outcome after paediatric cochlear implantation: diminution of complications with the evolution of new surgical techniques. J Otolaryngol. 2000 Oct;29(5):285–9.
[Pubmed]
12. Jiang Y, Gu P, Li B, Gao X, Sun B, Song Y, et al. Analysis and Management of Complications in a Cohort of 1,065 Minimally Invasive Cochlear Implantations. Otol Neurotol. 2017 Mar;38(3):347–51.
[Pubmed]| [Crossref]
13. Qiu J, Chen Y, Tan P, Chen J, Han Y, Gao L, et al. Complications and clinical analysis of 416 consecutive cochlear implantations. Int J Pediatr Otorhinolaryngol. 2011 Sep;75(9):1143–6.
[Pubmed] | [Crossref]
14. Halawani R, Aldhafeeri A, Alajlan S, Alzhrani F. Complications of post-cochlear implantation in 1027 adults and children. Ann Saudi Med. 2019;39(2):77–81.
[Pubmed] | [Crossref]