Case Report Published on December 20, 2023
An Endoscopic Transoral Approach to Parapharyngeal Space
Vinod Felix1, Lakshmi Anilkumar1, Anciya Beegom1
1. Department of Otorhinolaryngology, KIMSHEALTH, Trivandrum, Kerala*
ABSTRACT
Surgical approaches to parapharyngeal spaces are challenging and the selection of appropriate surgical approach is the key to successful operation. Literature regarding the endoscopic transoral approach to the parapharyngeal space is sparse. We present two different conditions of parapharyngeal space which were approached via an endoscopic transoral approach.
Keywords: Parapharyngeal Space (PPS), Endoscopic, Transoral
Introduction
One area of anatomy that is a true passage of secrecy is the anatomy of the potential anatomical spaces.1 Understanding the anatomy of parapharyngeal space is important in making a correct diagnosis and surgical plan for removing tumors in this region.1
Here we report 2 different cases of parapharyngeal space condition which were approached via an endoscopic transoral approach.
Case 1
A 10-year-old boy presented with 5 day history of fever, pain while swallowing, and pain on neck movements. On examination, he was found to have torticollis with his head turned to the right side (Cock Robin position). Blood investigations revealed a high total count with neutrophilic leukocytosis, high ESR, and CRP.
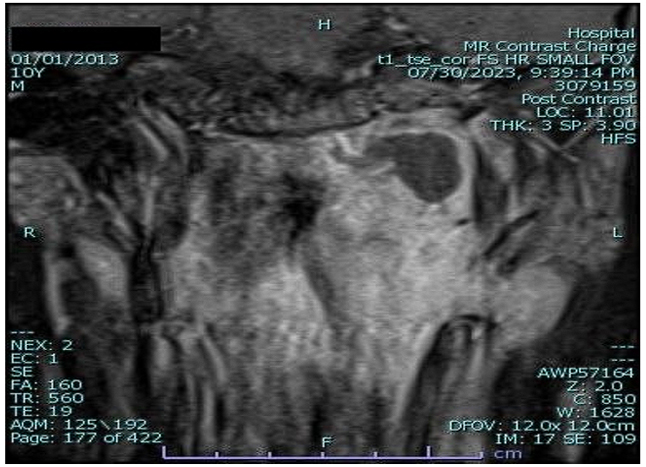
Figure 1. Showing MR neck of case 1
Contrast-enhanced computed tomography of the neck showed an irregular peripheral enhancing area with central non-enhancing components measuring 2.1*2.7*3cm on the left side of the level of nasopharynx extending from jugular foramen to C3 vertebrae and posteriorly up to prevertebral space (Figure 1).
The child was initially managed with parenteral antibiotics, steroids, and anticoagulants for 48 hours. Since the child had no symptomatic improvement after 48 hours of antibiotic therapy, a repeat scan was done and the abscess size remained the same. Hence, we proceeded with surgical abscess drainage via an endoscopic transoral approach (Figure 2,3,4). The post-operative period was uneventful; the child improved symptomatically and was discharged on postoperative day 2.

Figure 2. Showing the incision of case 1

Figure 3. Showing abscess in post styloid compartment with ICA (internal carotid artery) and SC (superior constrictor muscle) labelled in circle and triangle respectively
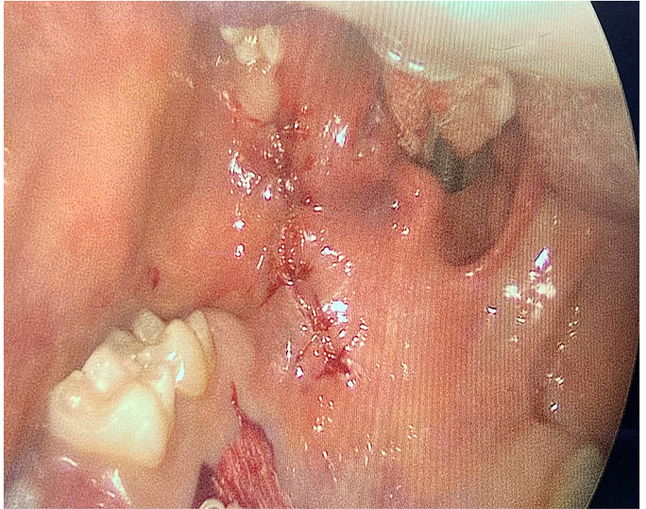
Figure 4. Shows closure of incision in case 1
Case 2
A 59-year-old male known case of subclinical hypothyroidism presented with a progressive increasing bulge left side of the throat, difficulty in swallowing, and a change in voice of 6 months duration. He also gives a history of left tonsillectomy with near total excision of supra tonsillar mass in March 2022 elsewhere (hpr- pleomorphic adenoma). On examination, he was found to have a hot potato voice and a mucosal bulge of the posterior end of the hard palate, entire soft palate, left anterior pillar, and left tonsillar fossa with a deviation of the uvula to right causing narrowing of about 40 % of the oropharyngeal isthmus.
MR neck showed a hyperintense space-occupying lesion measuring 6cm in length, 4.1cm in right to left width and 3.1 cm AP width noted left parapharyngeal space extending superiorly up to the floor of nasopharynx on the left side and inferiorly up to the level of the hypopharynx and closely abutting prevertebral muscles. Bulk involves the left oropharyngeal wall and tonsillar fossa. Intraluminal extension noted into the oropharynx crossing the midline along the posterior wall and causing luminal narrowing. The posteroinferior margin of the lesion closely abuts the left carotid sheath above the level of carotid artery bifurcation, the anterior margin laterally abuts the pterygoid muscles and the posterolateral margins abut deep lobe of the parotid gland with preserved fat planes (Figure 5). We approached the tumor trans orally with the use of an endoscope and it was removed completely (Figure 6,7). and a palatal island flap was used for the reconstruction of the soft palate. The post-operative period was uneventful.
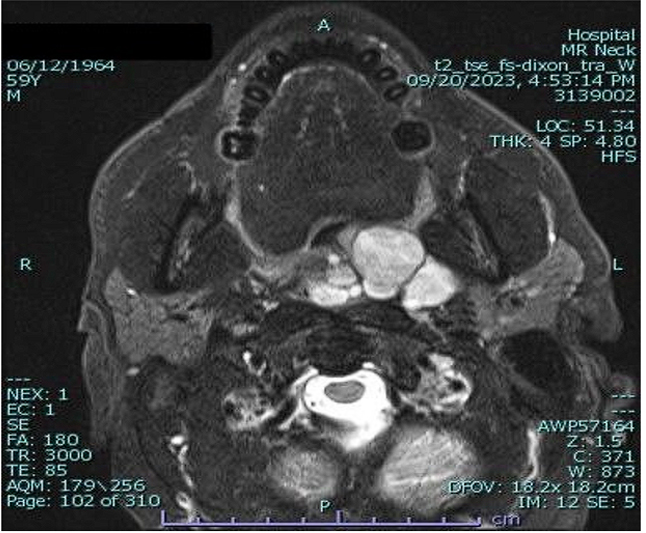
Figure 5. Showing MR neck of case 2
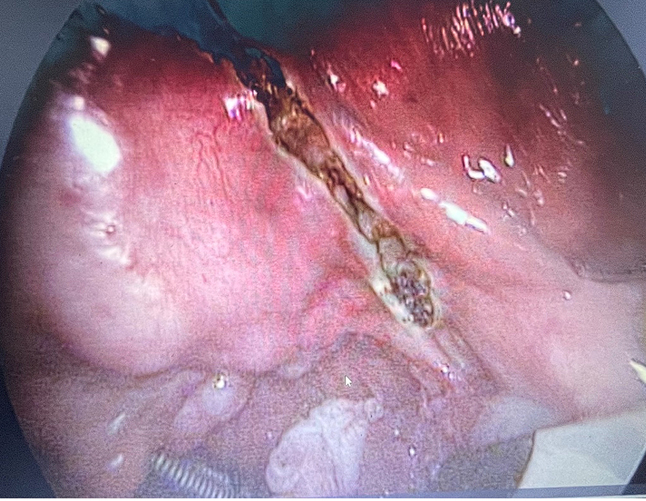
Figure 6. Showing incision of case 2 along with the tumour
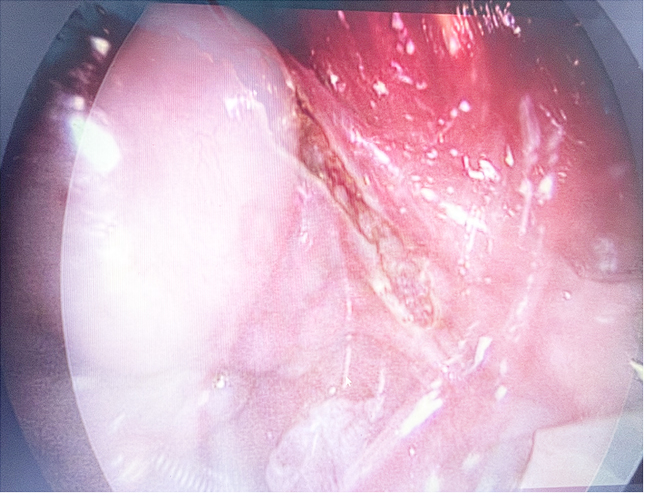
Figure 7. Showing the mass being dissected out
SURGICAL ANATOMY2
Patient positioned in a tonsillectomy position under general anesthesia with nasotracheal intubation. Boyle Davis mouth gag is inserted. An intraoral incision is made from the posterior edge of the hard palate passing along the lateral edge of the soft palate and medial edge of the palatoglossal arch. With the use of an endoscope, the mucosa, submucosa, and the superior constrictor muscles were identified and divided to enter the prestyloid space. The lateral boundary is the medial pterygoid muscle. The area between the medial pterygoid muscle and the superior constrictor muscle is the prestyloid space. Once the prestyloid space is cleared the styloid diaphragm and belly of styloglossus muscle becomes visible. The styloid diaphragm envelops the styloglossus muscle, stylopharyngeus muscle, and stylohyoid muscle. The pterygoid venous plexus lies in the space between the stylopharyngeus muscle and the superior constrictor muscle. The internal carotid artery, ascending pharyngeal artery, and ascending palatine artery are seen after removing the pterygoid plexus. The internal jugular vein lies lateral to the ICA. The cranial part of the hypoglossal nerve lies just on the medial aspect of ICA. The pharyngeal plexus lies in this area which is the anastomosis between the vagus nerve, hypoglossal nerve, and the cervical sympathetic chain. Between the IJV and ICA lies the initial exocranial portion of lower cranial nerves (IX through XI). The inferior and lateral boundaries of dissection are the greater cornua of hyoid bone and tendon of digastric muscle which lies medially and below styloglossus muscle respectively. The longus capitis muscle can be visualized by extending the dissection medially. At this level, there is no anatomic landmark that divides parapharyngeal space from retropharyngeal space. (Figure 8 shows the surgical anatomy)

Figure 8. Showing styloglossus muscle (SGM), stylopharyngeus muscle (SPM), superior constrictor muscle (SCM), ascending pharyngeal artery (APA), ascending palatine artery (APaA), facial artery (FA), parapharyngeal portion of internal carotid artery (ICAp), internal jugular vein (IJV), medial pterygoid muscle (MPM), glossopharyngeal nerve (IXcn), spinal accessory nerve (XIcn), hypoglossal nerve (XIIcn)
DISCUSSION
The parapharyngeal space is a pyramidal-shaped potential space filled with fat and areolar tissue extending superiorly from the skull base to the greater cornua of the hyoid bone inferiorly. It is also known as the pterygomaxillary space, pharyngomaxillary space, pterygopharyngeal space, and lateral pharyngeal space. The medial surface comprises of superior constrictor muscle, buccopharyngeal fascia, and the pharynx. The lateral surface comprises the medial pterygoid, the ramus of the mandible, and the deep lobe of the parotid gland. The posterior surface is a part of the prevertebral fascia bordered by the carotid sheath posterolaterally and the retropharyngeal space posteromedially. The PPS is divided into prestyloid and post-styloid compartments by the fascial condensation called the aponeurosis of Zuckerkandl and Testut, which joins the styloid process to the tensor veli palatini muscle. The prestyloid compartment contains adipose tissue, lymphatics, ectopic salivary gland tissue, a small branch of trigeminal nerve to tensor veli palatini, and branches of ascending pharyngeal artery and pharyngeal venous plexus. The post-styloid compartment is posteromedial and contains the ICA, IJV, cranial nerves IX to X11, the cervical sympathetic chain, lymph nodes, and glomus bodies.3
Surgical excision is the cornerstone for the treatment of PPS tumors, but the choice of the most adequate approach still represents a challenge because of the need to balance complete removal with the risk of morbidity.4
Many surgical approaches to PPS have been described but none of them completely fulfills the purposes of a complete tumor removal with low morbidity, minimal or no scars, and the preservation of surrounding nerves and vessels. Various approaches to parapharyngeal space include transcervical (most common), trans parotid, trans mandibular, transoral, and combined approaches.
The choice of surgical approach is dependent on tumor size, location, and proximity to important neurovascular structures. The transoral approach for parapharyngeal space has been criticized due to its restrictive exposure and increased rate of vascular and nerve injuries.5
The trans-oral approach was first described by Ehrlich in 1950 and was indicated for small nonvascular tumors.6
In 1988 Goodwin and Chandler advocated this approach to give adequate access to the parapharyngeal space. In their study of 6 cases there were no surgical complications and blood loss was minimal.7
The transoral approach is not an operation, but rather a method of exposure.7
When considering a transoral approach to removing a PPS mass preoperatively, a surgeon should consider multiple patient and tumor factors, including, but not limited to, cytopathology, the lateral and superior extent of the tumor, tumor relationship to the carotid artery and any trismus or limitation of neck flexion/extension.8
The advantages of the transoral approach include lack of external scar (cosmetically acceptable), minimally invasive, less morbidity and mortality, osteotomies can be avoided, no post-op neck drain, less intraoperative bleeding, less perioperative pain, early initiation of oral feed, shorter hospital stay, avoidance of neck numbness, eliminate first bite syndrome, diminishes the risk of cranial nerve injury and more over the use of endoscope provides magnification, illumination, angled view documentation, and teaching purpose.8,9,10
The disadvantages include limited exposure, dehiscence of incision, only one hand free of the surgeon, cannot be done in case of severe trismus and it has a learning curve.
CONCLUSION
PPS tumors have been approached earlier by transcervical or trans parotid approaches while the transoral route was reserved only for the treatment of small tumors of the prestyloid compartment. The horizons of a purely endoscopic transoral approach to PPS can be now widened to include even huge tumors and abscesses in prestyloid as well as post-styloid compartments, as an endoscope provides a magnified anatomical picture and is a safer option to work near the great vessels and nerves of PPS. The key to success remains in the proper knowledge of anatomy, knowledge of radio imaging, proper preoperative planning, and adequate hemostasis.
END NOTE
Author information
- Dr Vinod Felix, MBBS, MS
Senior Consultant ENT, Rhinology and Skull Base Surgery
KIMS Health, Trivandrum - Dr. Lakshmi A, MBBS, MS ENT
Senior Resident
Department of ENT
KIMS Health, Trivandrum - Dr. Anciya Beegom, MBBS, DLO
Junior resident
Kims Health, Trivandrum
Conflict of Interest: No conflict of interest
REFERENCES
- Macoveanu G, Costinescu VN, Hamarsheh AK. Parapharyngeal space-history and surgical study. Rev Med Chir Soc Med Nat Lasi 2011;115(3):820-825.
[Pubmed] - Dallan, Iacopo, Veronica Seccia, Luca Muscatello, Riccardo Lenzi, Paolo Castelnuovo, Maurizio Bignami, Filippo Montevecchi, Manfred Tschabitscher, and Claudio Vicini. “Transoral Endoscopic Anatomy of the Parapharyngeal Space: A Step-by-Step Logical Approach with Surgical Considerations.” Head & Neck 33, no. 4 (April 2011): 557–61.
[Pubmed] | [Crossref] - Krishnan S. Tumours of the parapharyngeal space. In: Scott – Brown’s Otorhinolaryngology Head & Neck Surgery,8th edn. Boca Raton: CRC press, 2018.
- Orlando, Pietro, Luca Giovanni Locatello, Oreste Gallo, Gianluca Leopardi, and Giandomenico Maggiore. “Endoscopy-Assisted Transoral Approach for Parapharyngeal Space Tumors: Our Experience and a Systematic Review of the Literature.” World Journal of Otorhinolaryngology - Head and Neck Surgery 9, no. 1 (March 2023): 79–90.
[Pubmed] | [Crossref] - Lao, Wilson P., Peter S. Han, Nathan H. Lee, Jason E. Gilde, and Jared C. Inman. “Transoral Excision of Parapharyngeal Tumors.” Ear, Nose, & Throat Journal 100, no. 10 (December 2021): NP454–58.
[Pubmed] | [Crossref] - Ehrlich, H. “Mixed Tumors of the Pterygomaxillary Space; Operative Removal; Oral Approach.” Oral Surgery, Oral Medicine, and Oral Pathology 3, no. 11 (November 1950): 1366–71.
[Pubmed] | [Crossref] - Goodwin WJ, Chandler JR. Transoral excision of lateral parapharyngeal space tumors presenting intraorally. The Laryngoscope, 1988;98(3):266-269.
[Crossref] - Larson, Andrew R., and William R. Ryan. “Transoral Excision of Parapharyngeal Space Tumors.” Otolaryngologic Clinics of North America 54, no. 3 (June 2021): 531–41.
[Pubmed] | [Crossref] - Fan S, Lin S, Zhang H, Li Q, Chen W, Wang Y, et al. A comparative study of endoscopy assisted transoral approach versus external approaches for the resection of large benign parapharyngeal space tumors. Oral Surg Oral Med Oral Pathol & Oral Radiol 2016; 123(2):157-162.
[Pubmed] | [Crossref] - Iseri, Mete, Murat Ozturk, Ahmet Kara, Selcuk Ucar, Omer Aydin, and Gurkan Keskin. “Endoscope-Assisted Transoral Approach to Parapharyngeal Space Tumors.” Head & Neck 37, no. 2 (February 2015): 243–48.
[Pubmed] | [Crossref]