Case Report Published on December 20, 2023
Rare Case of Nasal Polyp : Inflammatory
Myofibroblastic Tumor
Ihsan A T1, Vishnupriya Padmakumar1
1. Department of ENT, Jubilee Mission Medical College and Research Institute, Thrissur – 68 0005*
ABSTRACT
Inflammatory myofibroblastic tumor (IMT) is a rare tumor with a variable natural history and biologic behavior, ranging from completely benign to malignant with fatal outcome.1 It is an uncommon, presumably benign (non-cancerous) tumor made up of cells called myofibroblastic spindle cells.2
Keywords: Myofibroblastic Tumor, Nasal Cavity, Endoscopic Sinus Surgery, Cytokeratin
INTRODUCTION
Inflammatory myofibroblastic tumor (IMT) is an uncommon tumor that occurs most frequently in the lung, abdominal cavity, retroperitoneum, and extremities. Occurrence in the upper respiratory tract is uncommon but has been reported. It is now recognized as a neoplastic process that usually follows a rather benign clinical course after radical excision, but cases of invasive, locally recurrent, and metastatic forms have been reported.2
The diagnosis of IMT is difficult to establish before surgery because of its diversified radiologic manifestations. At one extreme, advanced disease is often misdiagnosed as a malignant tumor because of extensive infiltration and bony destruction.3 At the other extreme, it simulates various benign lesions in its earliest stage when it is confined to the mucosa.1
CASE REPORT
30 year old male presented to ENT OPD at Jubilee Mission Medical College with complaints of nasal block for years. There is history of recurrent nasal discharge, occasional headache and anosmia. Also gives past history of nasal surgery. Patient had no comorbidities.

Figure 1. Showing widening of dorsum of nose

Figure 2. Anterior rhinoscopy
On examination there was gross widening of external nose (Figure 1). Anterior rhinoscopy showed pale glistening mass seen completely filling both the nasal cavities (Figure 2). Posterior rhinoscopy revealed extension of mass lesion into the nasopharynx.
Computed Tomography of Paranasal sinuses (CT PNS) which was taken an year back from elsewhere showed haziness suggestive of a large polyp occupying the whole of right nasal cavity, both maxillary and ethmoid sinuses. Small polyp was seen in the left nasal cavity. Post procedural changes were seen. Orbital wall bony defect was noticed in both sides.
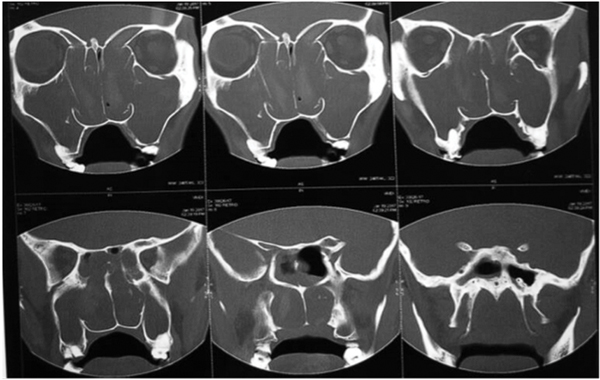
Figure. 3 CT PNS
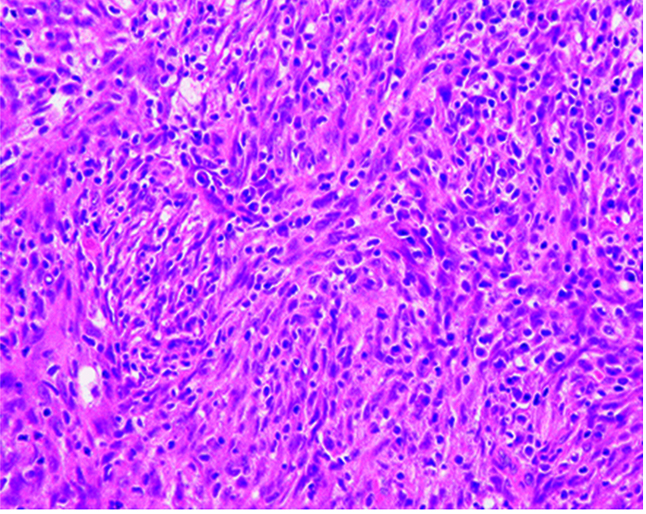
Figure. 4 Showing Spindled Myofibroblasts and Inflammatory Cells
Repeat CT (Figure 3) during his visit here revealed progression of lesion ending up filling both nasal cavities and showing haziness of all the sinuses.
Patient was posted for Endoscopic sinus surgery. Intraoperatively B/L extensive ethmoidal polyposis was seen. Polypoidal mucosa was seen in both maxillary antra and sphenoid and frontal sinuses. Same was cleared. Specimen was sent for HPE. Fungal stain was also sent which showed thin septate hyphae.
Histopathology report (Figure 4) came as inflammatory myofibroblastic tumor. Fungal culture showed no growth.
Immunohistochemistry was done to confirm the diagnosis (Positive stains: Cytokeratin (CK), Vimentin, SMA, CD68, Ki 67 proliferation index 3-5%). It was also mentioned that there is chance of recurrence and rarely tumor metastasis.Patient was given IV antibiotics, intranasal steroids and other supportive measure

Figure 5. On follow up
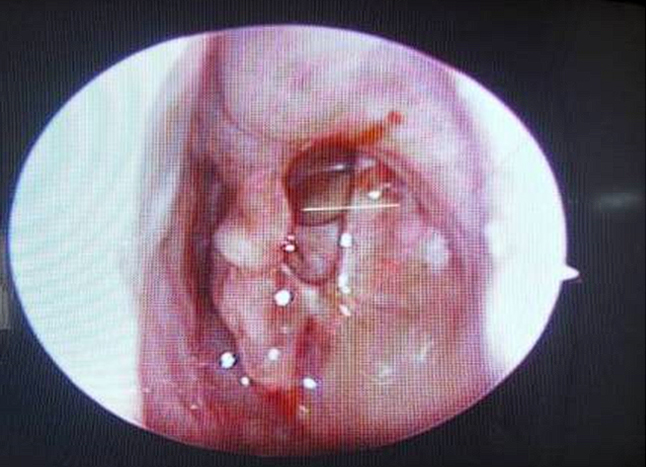
Figure 6. Post operative DNE finding
Post procedure Diagnostic Nasal Endoscopy (DNE) (after 1 week) was done which showed: healthy cavity. Raw bone showing charred appearance. Follow up DNE (after 2 weeks) showed thick mucoid discharge from all sinus opening – which was cleared. The charred appearance has changed to yellowish brown suggestive of healing. Follow up after 2 months showed no polyps in nasal cavities (Figure 5) and DNE was done which showed completely healed cavities (Figure 6).
DISCUSSION
IMT is a rare tumour with variable natural history and biological behaviour. It should be regarded as a soft-tissue mesenchymal tumor with low malignant potential, related to inflammatory fibrosarcoma. It is most commonly found in the lung, abdomen, retroperitoneum and extremities, and its occurrence in the head and neck region is less common. There is no age preference identified, with equal incidence in male and female patients.4 Whether individual IMT is a neoplastic or a reactive process is controversial, but at least a subset of IMT represents true neoplasia rather than reactive myofibroblastic proliferation.2
IMT is composed of spindled myofibroblasts and inflammatory cells (plasma cells, lymphocytes and eosinophils)
Signs and Symptoms
It varies depending on the site of the tumor. Some people with an IMT are asymptomatic, while others may have nonspecific respiratory symptoms, fever, or pain. IMTs may recur, and occasionally become locally invasive and/or spread (metastasize) to other parts of the body. The underlying cause of IMTs is poorly understood.1-4 Some cases have been linked to translocations involving the ALK gene.5
The underlying cause of inflammatory myofibroblastic tumors (IMTs) remains unknown. While some researchers believe it is a true neoplasm, others believe that it represents an immunologic response to an infectious or noninfectious agent
Treatment
Treatment is mainly surgical resection. Other treatment modalities are corticosteroids, radiotherapy, chemotherapy.7
Prognosis
In general, inflammatory myofibroblastic tumors (IMTs) follow a benign course with a favorable outcome after they are surgically removed. In some cases, they can be invasive, recur locally, or spread (metastasize).7 A metastatic IMT has a poorer prognosis and can cause death.3 An IMT can also be indolent, with prolonged survival despite multiple recurrences. Rearrangements of genetic material involving the ALK gene are present in the tumor in some affected people (known as being ALK-positive). Being ALK-positive may be associated with a more favorable prognosis. One study found that a higher percentage of patients with localized disease were ALK-positive (about 60%) compared to those with multicentric (having 2 or more separate growths) IMTs (about 33%).
End Note
Author Information
- Dr Ihsan A.T., M.S., Professor, Department of ENT, Jubilee Mission Medical College and Research Institute, Thrissur
- Dr Vishnupriya Padmakumar, M.S ENT, DNB, Senior Resident, Department of ENT, Jubilee Mission Medical College and Research Institute, Thrissur
Conflict of Interest: None to declare
REFERENCES
- Lai V, Wong Yc, Lam Wy, Tsui Wc, and Luk Sh. “Inflammatory Myofibroblastic Tumor of the Nasal Cavity.” AJNR. American Journal of Neuroradiology. 2007 Jan 1;28(1):135-7.
[Pubmed] - Palaskar S, Koshti S, Maralingannavar M, Bartake A. Inflammatory myofibroblastic tumor. Contemporary clinical dentistry. 2011 Oct;2(4):274.2. Palaskar S, Koshti S, Maralingannavar M, Bartake A. Inflammatory myofibroblastic tumor. Contemporary clinical dentistry. 2011 Oct;2(4):274.
[Pubmed] | [Crossref] - Kovach, Stephen J., Anne C. Fischer, Philip J. Katzman, Rabih M. Salloum, Stephen E. Ettinghausen, Ralph Madeb, and Leonidas G. Koniaris. “Inflammatory Myofibroblastic Tumors.” Journal of Surgical Oncology 94, no. 5 (October 1, 2006): 385–91.
[Pubmed] | [Crossref] - Coffin, Cheryl M., Jason L. Hornick, and Christopher D. M. Fletcher. “Inflammatory Myofibroblastic Tumor: Comparison of Clinicopathologic, Histologic, and Immunohistochemical Features Including ALK Expression in Atypical and Aggressive Cases.” The American Journal of Surgical Pathology 31, no. 4 (April 2007): 509–20.
[Pubmed] | [Crossref] - Rosai J. Rosai and Ackerman’s Surgical Pathology E-Book. Elsevier Health Sciences; 2011.
- Mills SE, Carter D, Greenson JK, Reuter VE, Stoler MH. Sternberg’s Diagnostic Surgical Pathology. Lippincott Williams & Wilkins; 2012.
- Hansen, Chase C., Colby Eisenbach, Carlos Torres, Suzanne Graham, and Fred Hardwicke. “Maxillary Sinus Inflammatory Myofibroblastic Tumors: A Review and Case Report.” Case Reports in Oncological Medicine 2015 (2015): 953857.
[Pubmed] | [Crossref]