Original Reasearch Published on December 20, 2023
Vocal Fold Cysts: An Analysis of Flexible Fibreoptic Laryngoscopic Findings
Anjana John1
- Registrar and Fellow in Laryngology, Dr Jayakumar’s Institute of Laryngology, Thiruvananthapuram*
ABSTRACT
Vocal fold cysts are benign laryngeal lesions, which affect both children and adults. Diagnosis is by flexible laryngoscopy and videostroboscopy. This study is a retrospective analysis of videos of flexible laryngoscopic findings of 84 cases of vocal fold cysts. In our study, majority of patients were in adult age group. On flexible laryngoscopy, almost all of the cysts were unilateral .Most common site of origin was the medial margin of the vocal folds. Thin walled and thick walled cysts were almost equal in number. On stroboscopic examination, mucosal waves were absent over the cyst in all cases. Hourglass shaped phonatory gap was most commonly seen. Ventricular band hyperadduction (Type 2 MTD) was seen commonly as a compensatory maneuver. Interarytenoid pachydermia was present in around 70 % patients which indicates a high association of laryngopharyngeal reflux with vocal fold cyst.
INTRODUCTION
Vocal fold cysts are benign laryngeal lesions, which affect both children and adults. They are subepithelial and can be either unilateral or bilateral. Histologically they are classified into mucus retention cysts and epithelial inclusion cysts. Diagnosis is by flexible laryngoscopy and videostroboscopy. Surgery is the definitive treatment for symptomatic vocal fold cysts (Figure 1).
MATERIALS AND METHODS
This is a retrospective study. We reviewed the recorded videos of flexible laryngoscopy of 84 cases of vocal fold cysts in patients who attended Laryngology OPD in Dr Jayakumar’s Laryngology Clinic during the period from 2009 to 2020. Flexible laryngoscopic findings such as side of lesion, thin or thick walled cyst, stroboscopic findings of mucosal waves and phonatory gap, presence of contact lesions or other associated lesions, compensatory maneuvers like ventricular band hyperadduction and anteroposterior compression, status of arytenoids, and presence of interarytenoid pachydermia indicating laryngopharyngeal reflux were studied.
RESULTS AND ANALYSIS
Age:
Of the 84 patients, 82 (97.62 %) were adults while 2 (2.38 %) were of pediatric age group. Of the 2 pediatric cases, one had bilateral vocal fold cyst (Table 1).
Sex:
51 (60.71 %) were male patients, while 33 (39.29 %) were females. Male: female ratio is 1.55: 1 (Table 2).
Unilateral or Bilateral:
Unilateral cyst were seen in 79 cases (94.05 %) while bilateral cysts in 7 cases (5.95 %) (Table 3) (Figure 2).
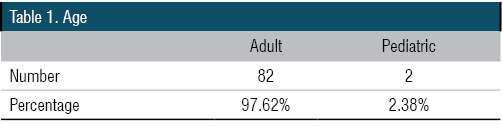
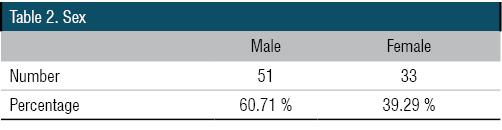


Figure 1. Right VC Cyst
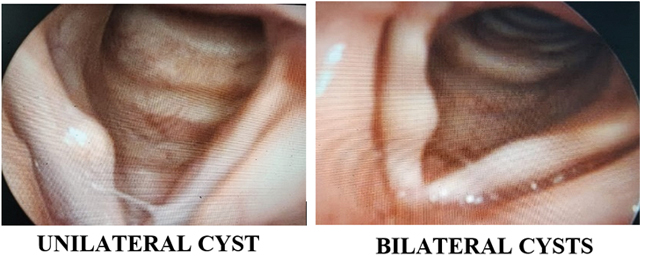
Figure 2. Unilateral Cyst and Bilateral Cyst
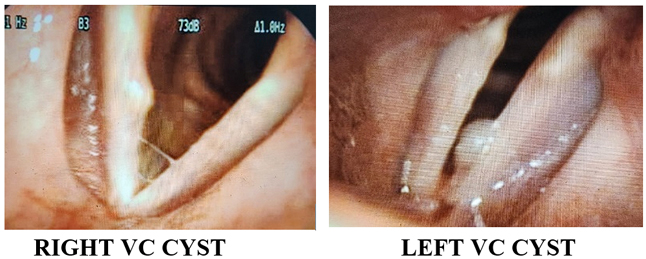
Figure 3. Right VC Cyst, Left VC Cyst
Side Involved:
Of the 79 cases of unilateral cysts, 42 (53.16 %) occurred on right side and 37 (46.84 %) on left side (Table 4) (Figure 3).
Site of involvement in the Vocal Fold:
In 61 patients (72.62 %), cysts were found in the medial margin of vocal folds, while in 17 patients (20.24 %) on superior surface and in 6 patients (7.14 %) cysts arose from inferior lip (Table 5) (Figure 4).
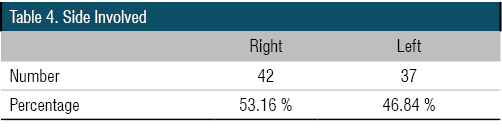

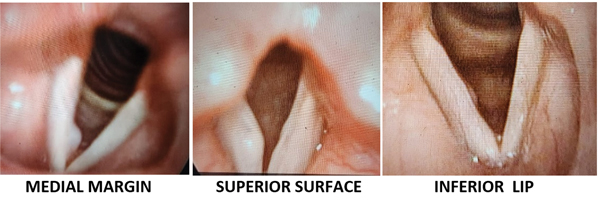
Figure 4. Site of Involvement
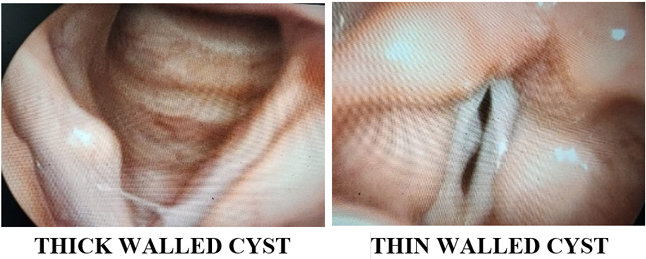
Figure 5. Thick Walled or Thin Walled Cyst
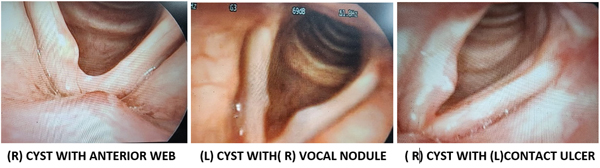
Figure 6. Associated Lesions
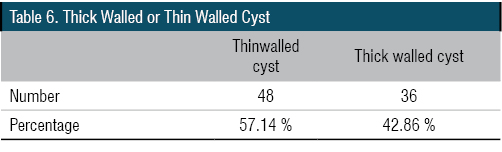
Thick walled or Thin Walled Cyst:
48 (57.14 %) cases of cysts appeared to be thin walled while 36 (42.86 %) cases of cysts appear thick walled (Table 6) (Figure 5).
Contact Lesions and Associated Lesions:
Contact lesions included 1 case of vocal nodule and 1 case of vocal polyp.
In 16 patients, there were associated lesions which included 3 cases of sulcus vocalis, 2 cases each of contact ulcer, unilateral vocal fold paresis, bilateral vocal fold immobility and ventricular prolapse and 1 case each of bilateral submucosal hemorrhage, anterior microweb, vocal polyp, vocal nodule and presbylarynx (Table 7,8) (Figure 6,7).
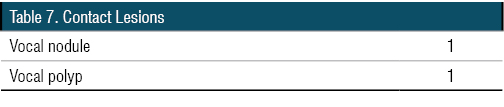
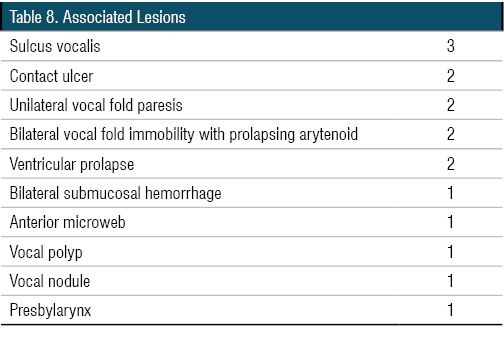

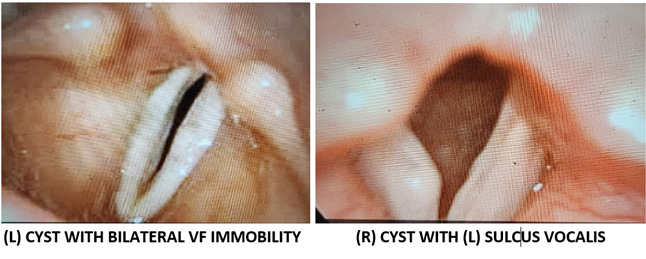
Figure 7. Associated Lesions
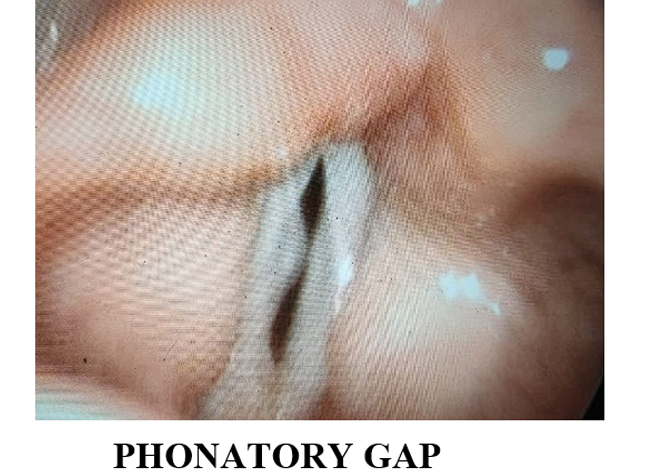
Figure 8. Phonatory Gap
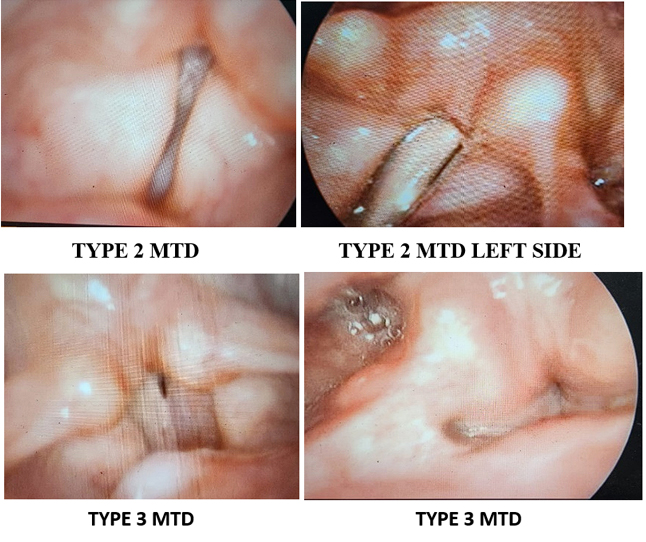
Figure 9. Compensatory Maneuvers
Recurrence:
1 case of recurrence of cyst following spontaneous resolution was also seen.
Mucosal waves on Stroboscopy:
On stroboscopic examination mucosal waves over the cyst was absent in all cases.
PHONATORY GAP:
On saying ‘ee’, phonatory gap was noticed in 64 patients, while there was no or minimal gap in 20 patients (Figure 8) (Table 9).
Of the 20 patients with no phonatory gap, cyst was located in superior surface in 9 cases, medial margin in 7 cases and inferior lip in 4 cases.
COMPENSATORY MANEUVERS:
Compensatory maneuvers included Type 2 MTD (ventricular band hyperadduction) seen in 30 patients, Type3 MTD seen in 7 patients of which there was anteroposterior compression in 4 patients and posterior displacement of epiglottic tubercle in 3 patients (Table 10) (Figure 9).


Figure 10. Overriding of Left Arytenoid
STATUS OF ARYTENOIDS:
Movement of arytenoids was examined to see if there was any over riding on phonation.
Overriding of arytenoids was seen in some patients, maybe as a normal phenomenon or as part of a compensatory maneuver for better closure of phonatory gap.
Overriding of arytenoids on phonation was seen in 46 patients (Table 11) (Figure 10).
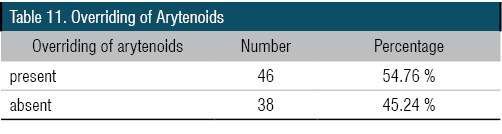
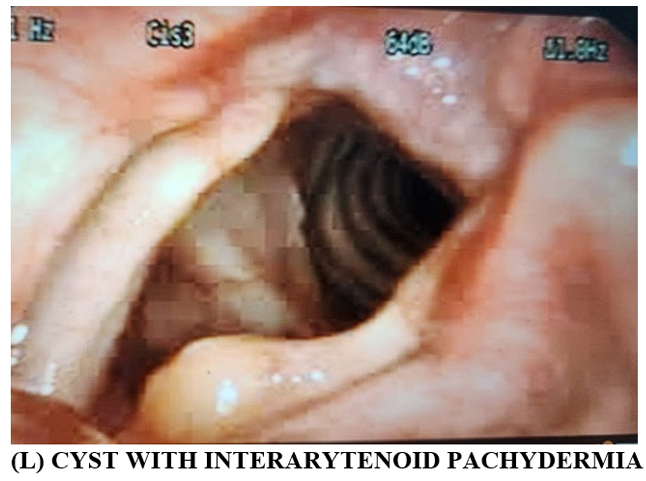
Figure 11. (L) Cyst with Interarytenoid Pachydermia

Presence of Interarytenoid Pachydermia :
Presence of interarytenoid pachydermia suggestive of laryngopharyngeal reflux was present in 59 patients (Table 12) (Figure 11).
DISCUSSION
The human vocal folds have a unique microanatomy. Histologically, the vocal folds consist of five layers -squamous epithelium, superficial, intermediate and deep layers of lamina propria and the vocalis muscle. According to the cover body theory of vocal fold motion as proposed by Hirano in 1974, the epithelium and superficial layer of lamina propria forms the ‘cover’ while the intermediate and deep layers of lamina propria comprise the ‘transition’ layer and the vocalis muscle acts as the ‘body’. As air passes between the vocal folds, the loose cover moves in a wave like motion over the stiffer body.
A cyst is a benign, well encapsulated collection of fluid of varying consistency. Vocal fold cyst is typically found in the superficial layer of lamina propria. Usually the cyst lies free under the epithelium. Sometimes it may be adherent to the overlying epithelium or it may open into the laryngeal lumen or it may extend into the vocal ligament. Histologically, they can be mucus retention cysts or epidermoid cysts.
In mucus retention cysts, the lining is much thinner and it is made of respiratory epithelium and it contains clear or yellow fluid. It is the result of occlusion of mucus glands on the vocal folds. This occlusion may be due to phonotrauma resulting in thickened epithelium usually at the junction of anterior one third and posterior two third of medial margin of membranous cord or due to infection. Due to presence of a thin wall, these cysts usually rupture during surgical excision.
In epidermoid cyst, the lining is thicker and made of stratified squamous epitheliumand it contains thick pultaceous often cheesy material containing keratin and cholesterol debris. They are believed to be congenital, constituting remnants of fourth and sixth branchial arches. They may also arise from phonotraumatic fissures developing on the vocal fold epithelium with ingrowth of some epithelium into SLP. The epidermoid cysts are usually seen on the superior surface of the vocal fold at the striking zone. Because of the thick wall they usually do not rupture during surgical excision.
Patient with vocal fold cyst will usually present with a hoarse voice. Sometimes voice maybe rough and breathy if coexistent sulcus is present.
On videostrobosopic examination, mucosal waves appear reduced or absent and hour glass pattern of glottic closure is usually seen.
Patients with vocal fold cysts usually develop bad compensatory techniques which includes ventricular band hyperadduction and anteroposterior compression. The opposite vocal fold may develop a contact lesion occasionally.
Surgery involves excision of cyst with cold steel phonomicrosurgical instruments with or without the aid of laser. Following subepithelial infiltration, a lateral mini microflap incision is put. Cyst is gently dissected from the SLP and overlying epithelium. Anterior and posterior fibrotic bands are cut sharply and cyst removed trying to preserve the infraglottic epithelium as much as possible. If cyst wall breaks, an attempt is made to remove the entire cyst wall if possible, to prevent recurrence.
In our study which included 84 cases of vocal fold cysts, majority of patients were in adult age group. Of the 2 pediatric patients, one had bilateral vocal fold cyst. Male: female ratio was 1.55:1. Analysis of flexible laryngoscopic findings showed that almost all of the cysts were unilateral, of which 53.16% occurs on right side. Most common site of origin was the medial margin of the vocal folds, while some cysts arose from superior surface and inferior lip. Thin walled and thick walled cysts were almost equal in number with slight preponderance of thin walled cysts. Although contact lesions were few, associated lesions like sulcus vocalis, unilateral and bilateral vocal fold immobility, vocal cord polyp and nodule, contact granuloma, ventricular prolapse, submucosal hemorrhages and presbylarynx were seen. On stroboscopic examination, mucosal waves were absent over the cyst. Hourglass shaped phonatory gap was seen in most cases. Most common compensatory maneuver seen was ventricular band hyperadduction (Type 2 MTD) though a few cases of anteroposterior compression and posterior displacement of epiglottic tubercle (Type 3 MTD) were seen. Half of the patients showed over riding of arytenoids on phonation. Overriding of arytenoids might have been a normal phenomenon or a part of a compensatory maneuver for better closure of phonatory gap. Interarytenoid pachydermia was present in around 70 % patients which showed that majority of patients with vocal fold cyst also suffered from Laryngopharyngeal reflux disease (LPRD).
CONCLUSION
Vocal fold cysts are benign laryngeal lesions which can cause hoarseness. It is diagnosed by flexible laryngoscopy and stroboscopy. In our study of analysis of flexible laryngoscopic findings of cases of vocal fold cysts, we found out that cysts are usually unilateral, occurring in medial margin of vocal folds. Cysts can be thin or thick walled. Contact lesions and other benign vocal fold lesions may be seen associated with it. Bad compensatory maneuvers like type 2 and type 3 MTD are seen. Most of the patients had associated features of LPRD. So besides surgery, good vocal hygiene, adequate hydration, treatment of reflux and postoperative voice therapy play a major role in management.
End Note
Author Information
- Dr Anjana John, MS ENT, Registrar and Fellow in Laryngology, Dr Jayakumar’s Institute of Laryngology, Thiruvananthapuram
Conflict of Interest: None to declare
REFERENCES
- Nerurkar N, Shukla S. Subepithelial vocal fold cysts: a pearl on a string? Int J LaryngolPhonosurg. 2012;2(2):53-6.
[Source] - Cipriani NA, Martin DE, Corey JP, Portugal L, Caballero N, Lester R, et al. The clinicopathologic spectrum of benign mass lesions of the vocal fold due to vocal abuse. Int J SurgPathol. 2011 Oct. 19(5):583-7.
[Crossref] - Bouchayer M, Cornut G, Witzig E, et al. Epidermoid cysts, sulci and mucosal brides of true vocal cord: a report of 157 cases. Laryngoscope. 1985;95(9 Pt 1):1087-94.
- Zeitels SM. Chapter 7: Benign lesions of the vocal folds. In: Fried MP, Tan- Geller M(Eds). Clinical Laryngology: The Essentials. Stuttgart: Thieme; 2014.pp. 56-73.
- Moore BA, Ossoff RA, Courey MS. Cysts, nodules and polyps. In: Ossoff RH, Shapshay SM, Woodson GE, Netterville JL(Eds). The Larynx. Philadelphia: Lippincott Williams & Wilkins; 2003.pp. 185-201.
- Monday LA, Cornut G, Bouchayer M, et al. Epidermoid cysts of vocal cords. Ann OtolRhinol Laryngol.1983;92:124-7
[Pubmed] | [Crossref] - Jensen, Jane Bjerg, and Niels Rasmussen. “Phonosurgery of Vocal Fold Polyps, Cysts and Nodules Is Beneficial.” Danish Medical Journal 60, no. 2 (February 2013): A4577.
[Pubmed]
- Tibbetts KM, Dominguez LM, Simpson CB. Impact of Perioperative Voice Therapy on Outcomes in the Surgical Management of Vocal Fold Cysts. J Voice. 2018 May. 32 (3):347-51.
[Pubmed] | [Crossref] - Timothy D, Anderson MD, Chapter 24: Benign lesions of the larynx. In: Merati AL, Bielamowicz SA (Eds). Textbook of Laryngology.San Diego,CA:Plural Publishing, Inc;2006.pp.303-22.
- Courey MS, Gardner GM, Stone RE, et al. Endoscopic vocal fold microflap: a three-year experience. Ann OtolRhinolLaryngol. 1995 Apr. 104(4 Pt 1):267-73.
[Pubmed] | [Crossref] - Hoffman, Henry T., Jonathan M. Bock, Lucy Hynds Karnell, and Janice Ahlrichs-Hanson. “Microendoscopy of Reinke’s Space.” The Annals of Otology, Rhinology, and Laryngology 117, no. 7 (July 2008): 510–14; discussion 515-516.
[Pubmed] | [Crossref] - Bouchayer, M., G. Cornut, E. Witzig, R. Loire, J. B. Roch, and R. W. Bastian. “Epidermoid Cysts, Sulci, and Mucosal Bridges of the True Vocal Cord: A Report of 157 Cases.” The Laryngoscope 95, no. 9 Pt 1 (September 1985): 1087–94.
[Pubmed] - Shvero, J., R. Koren, T. Hadar, E. Yaniv, J. Sandbank, R. Feinmesser, and R. Gal. “Clinicopathologic Study and Classification of Vocal Cord Cysts.” Pathology, Research and Practice 196, no. 2 (2000): 95–98.
[Pubmed] | [Crossref]