Original Reasearch Published on December 20, 2023
Vertigo Clinic - Our Departmental Experience
Rajesh Raju George1, Dhanya E K1, Abhin Lazer1, Swetha1, Ahana1
1. Department of ENT, Rajagiri Hospital, Aluva*
ABSTRACT
Vertigo, dizziness, unsteadiness, and falls are common symptoms encountered in day-to-day practice. Detailed evaluation of these symptoms is necessary for arriving at the correct diagnosis. Vertigo clinics equipped with videonystagmography help in the correct diagnosis and management of these patients.
Aims and Objectives: 1. To elaborate on the age and gender prevalence of patients attending the vertigo clinic 2. To elaborate on the different causes of vertigo encountered in vertigo clinics and to find out which is the commonest cause 3. Subclassify BPPV and find out the prevalence of different types of BPPV. 4. To throw light on the corrective maneuvers employed for different types of BPPV and the success rate of corrective maneuvers employed for different types of BPPV 5. To elaborate on non-BPPV causes of vertigo seen in our vertigo clinic.
Materials and Methods: A retrospective study was conducted on the patients who attended the Rajagiri vertigo clinic from 3/5/21 to 3/5/22. The patients who attend the vertigo clinic of Rajagiri Hospital follow the Departmental protocol which is discussed in detail. Statistical analysis was done using the Chi-square test.
Results: The patients who attended our vertigo clinic were mainly females. BPPV was the commonest cause of vertigo accounting for 85.425 % of cases of vertigo. BPPV was mainly posterior canal, lateral canal, and anterior canal of which the commonest was posterior canal followed by lateral and anterior. Corrective maneuvers employed was Epley’s for posterior canal BPPV, Barbeque roll for lateral canal BPPV, and Yacovino / Banglore maneuver for anterior canal BPPV whose success rate were 98%, 99%, and 100% respectively. Non-BPPV cases included central and peripheral causes. Vertigo clinics improve the diagnosis and management of vertigo.
Introduction
Vertigo clinics with videonystagmography have taken the diagnosis and management of vertigo a leap ahead. Rajagiri Hospital is a Tertiary care center equipped with a Vertigo clinic and videonystagmography. Vertigo, dizziness, and falls can be due to central causes, peripheral causes, cardiac causes, functional causes, diseases causing loss of physical strength, electrolyte imbalance, etc. Hence a detailed evaluation is needed to know the exact etiology and proper management. Vertigo clinics equipped with videonystagmography help in a comprehensive evaluation. This retrospective study done at Rajagiri Hospital for 1 year is based on the data of vertigo patients who were evaluated at Rajagiri vertigo clinic following the departmental protocol. Every day patients with vertiginous symptoms present to the emergency department, department of otorhinolaryngology, department of neurology, department of cardiology, department of General medicine, and all allied specialties. Because of teamwork and proper interdepartmental coordination, all the difficult cases of vertigo could be channelized through the vertigo clinic run by the Department of Otorhinolaryngology.
Aims and Objectives
- To elaborate on the age and gender prevalence of patients attending the vertigo clinic
- To elaborate on the different causes of vertigo encountered in vertigo clinics and to find out which is the commonest cause
- Subclassify BPPV and find out the prevalence of different types of BPPV.
- To throw light on the corrective maneuvers employed for different types of BPPV and the success rate of corrective maneuvers employed for different types of BPPV
- To elaborate on non-BPPV causes of vertigo seen in our vertigo clinic.
Materials and methods
A retrospective study was conducted on the patients who attended the Rajagiri vertigo clinic from 3/5/21 to 3/5/22. The departmental protocol was followed for the evaluation of patients with vertigo (Figure 1). From our records, we obtained the total number of patients who attended the vertigo clinic, their age, gender, whether they underwent a position test with Frenzel, whether the position test was positive for BPPV, corrective maneuver employed, a result of repeat position test done after one week of first corrective maneuver, the number of patients who underwent videonystagmography, the provisional diagnosis of the patients, how the patients were managed and their follow up .707 patients were evaluated in vertigo clinic in the last 1 year. 592 patients were positive for Benign Paroxysmal Positional Vetigo.115 patients underwent videonystagmography who had a diagnosis other than BPPV which is elaborated subsequently. Selection criteria for BPPV evaluation and videonystagmoraphy were as per department protocol devised for evaluation of vertigo which is as follows (Figure 1).
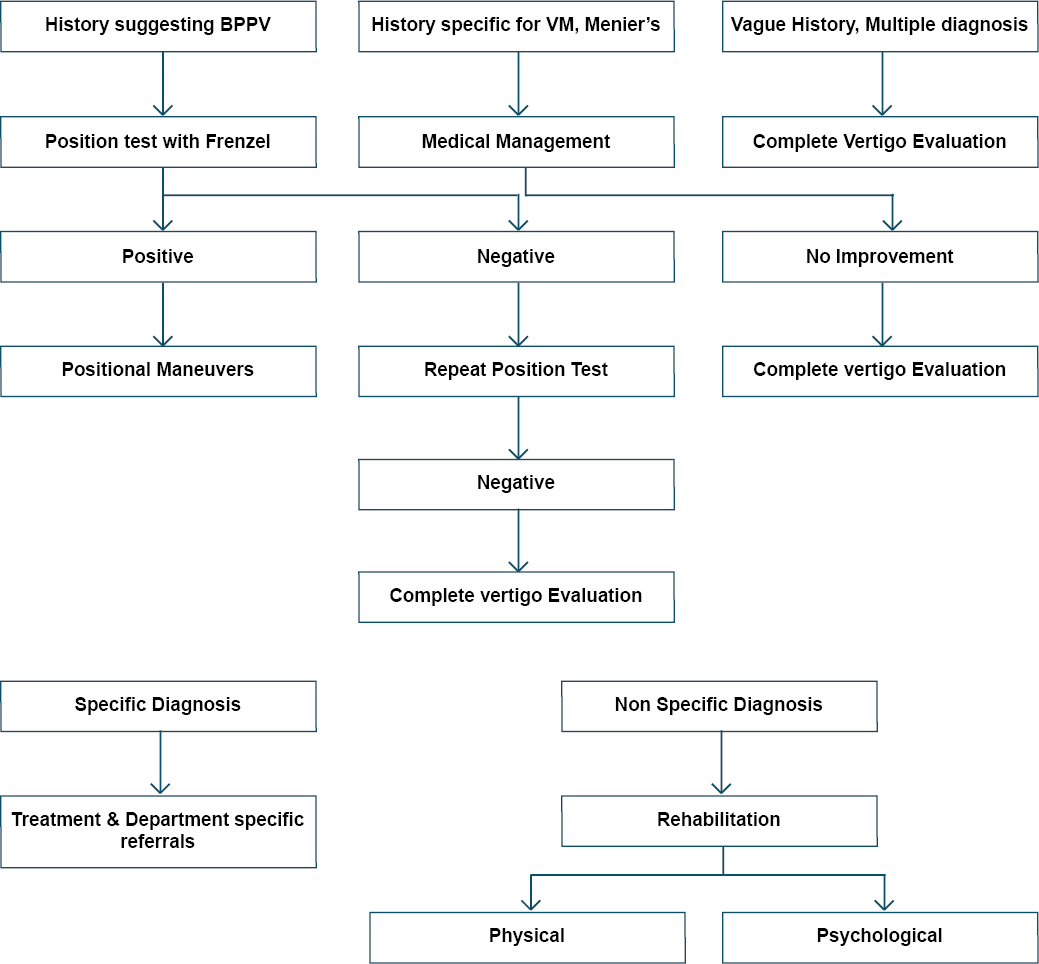
Figure 1. Departmental protocol for Evaluation of Vertigo

Figure 2. Distribution of Vertigo based on Gender
The protocol followed for the evaluation of vertigo was that any patient presenting with symptoms suggesting BPPV should be subjected to a position test with Frenzel and managed accordingly. If the position test with Frenzel was negative even after performing it under the correct circumstances, a complete evaluation is done in the vertigo clinic. In patients with vague symptoms, a history not very specific for a particular disease complete evaluation is done in the vertigo clinic. If the patient’s history points to a diagnosis like vestibular migraine, Meniere’s patient is given the proper treatment, and if there is not much improvement complete evaluation is done.
Position test with Frenzel is performed in the following way. Mcclure Pagnini test is performed first where the patient is made to sit straight with the leg in extension, and Frenzel glass is secured in place. Brought supine with the head flexed 30 degrees with the horizontal. The pattern of nystagmus and symptoms of vertigo are noted. The pattern of nystagmus generated during Mcclure right and left with the reversal of nystagmus if present is noted and recorded. If the test is positive 360-degree barbeque roll is employed for correction after identifying the type and side of horizontal canal BPPV correctly. The patient is asked to review the next week. If symptoms persist, a repeat position test with Frenzel is done, and if still positive a repeating roll is done.
Dix Hall pike test with Frenzel glass is done after performing Mcclure. After securing the frenzel glass, the neck is turned to one side by 45 degrees, the patient is brought to a supine position with the neck extended 30 degrees. Nystagmus generated is noticed and the patient is asked whether they get symptoms of vertigo. The reversal of nystagmus is noticed while the patient is brought back to the sitting position. Epley’s maneuver was used for correction routinely.
Anterior canal BPPV was diagnosed with a deep head hanging test. Downbeat nystagmus with torsion along with vertigo symptoms is interpreted as a positive deep head hanging test. A deep head hanging test was performed in cases that showed downbeat nystagmus during Dix Hall pike or Mcclure or in patients with a history typical for anterior canal BPPV. Mcclure Pagnini and Dixhallpike were routinely performed in all patients. For the anterior canal, BPPV Banglore /Yacovino maneuvers were employed to correct vertigo. Banglore maneuver for correction of anterior canal BPPV starts with the patient sitting in knee down position. Then go down with the forehead touching the ground. Hold for one minute or till vertigo subside. Then again bend the head so that the vertex touches the ground. Hold for one minute or till the vertigo subside. Then the patient is suddenly brought back to a sitting position. For patients who were finding it difficult to perform the Banglore maneuver, the Yacovino maneuver was employed.
In the Yacovino maneuver patient is made to sit with the leg in extension brought back to supine with the neck in extension. The patient is held in that position for 1 minute or till the vertigo subsides. The neck is flexed so that the chin touches the sternum. The patient is held in that position for one minute or till the vertigo subsides. Then the patient is brought back to a sitting position.
Those patients who were selected to be evaluated in the vertigo clinic with videonystagmography were studied in detail in a step-wise pattern. Vertigo evaluation starts with a detailed history which forms the crucial step. Physical examination is done in detail with the pulse rate which is recorded for one full minute in the supine and standing position. Any bradycardia or arrhythmia can be picked up. Blood pressure is recorded in the supine position and 3 minutes after standing. Making use of the principle of escalation of sensory denial patient’s ability to stand on a firm surface and soft surface with eyes open and closed is assessed and inferences are noted. A basic neurological evaluation was made. Tandem walking, test for dysdiadochokinesia, finger nose test to assess Cerebellar dysfunction, retropulsive pull test, test for suppression of Vestibular ocular reflex, Fukuda test, test for fine touch and temperature, vibration sense, head impulse test are performed routinely for each patient. The physical strength of the patient is assessed by Fullerton Advanced Balance Scale. Every patient’s emotional health is assessed with Hospital Anxiety and Depression Score. After these tests, Videonystagmography is done.
Sample Size
All patients who were evaluated in the vertigo clinic from 3/5/2021 to 3/5/2022. Data was entered in Microsoft Excel and analysed using SPSS V 25. Association between categorical variables was assessed using Chi Square test and T test was used to compare quantitative variables. A p value of < 0.05 was considered significant.
Results and Analysis
In the last year, 707 patients were evaluated in the vertigo clinic, of which 98.01% of vertigo cases were due to peripheral causes and 1.98% were due to central causes. Mean age of the study population was 59.60 ± 14.6 years. A brief description of the demographics, symptoms, comorbidities are given (Figure 2 – 5).

Figure 3. Main symptoms of patients attending the vertigo clinic
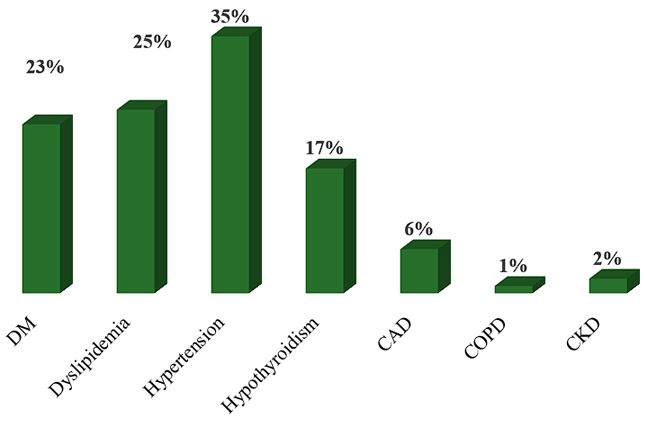
Figure 4. Comorbidities seen in patient’s attending the vertigo clinic

Figure 5. Side commonly involved in BPPV
Of the peripheral causes of vertigo, BPPV formed the major chunk occupying 85.42% of all cases followed by vestibular migraine accounting for 6.34% of cases. Vestibular migraine Meniere’s overlap syndrome (3.4%) was seen more than Meniere’s disease (1.73%). Vestibular neuronitis (0.86%), PPPD (0.8%), vestibular paroxysmia (0.57%), and unsteadiness due to lack of physical strength (0.72%) were other cases encountered.
Central causes seen in our vertigo clinic were Transient ischemic attacks accounting for 57.14% of cases, followed by stroke (21.42%). 7.14% of patients evaluated for unsteadiness turned out to be due to normal pressure hydrocephalus and 7.14% were detected to have progressive supranuclear palsy. We encountered bilateral CP angle arachnoid cyst as a cause of recurrent vertigo, accounting for 7.14%.
While evaluating BPPV, posterior canal BPPV formed the major chunk 51.68% followed by lateral canal and anterior canal. Of the lateral canal BPPV geotropic was the major cause accounting for 61.4% followed by apogeotropic type at 38.4%. Epley’s maneuver was employed for the correction of posterior canal BPPV. 98% of patients were corrected with single Epley’s. 2% of patients needed repeat Epley. For the horizontal canal, BPPV 360-degree barbeque roll was done for correction after identifying the type and side with accuracy. 99 % of patients were corrected in a single roll. 1 % needed repeat roll. For the anterior canal, the BPPV Banglore maneuver was employed for correction. For those who found it difficult to perform Banglore maneuver Yacovino maneuver was employed. 100% results were obtained for the Banglore maneuver and Yacovino maneuver (Figure 6).

Figure 6. Percentage of patients corrected by single corrective maneuver
Association of canal involvement with Age and Gender
Chi square test was done – and the association of gender with the type of canal involved was not significant with p value > 0.05 (Figure 7).
An Independent t test was done to assess the association of age with the location of the canal involved – No significant association was obtained (p value > 0.05) (Figure 8).

Figure 7. Association of Gender with canal involvement
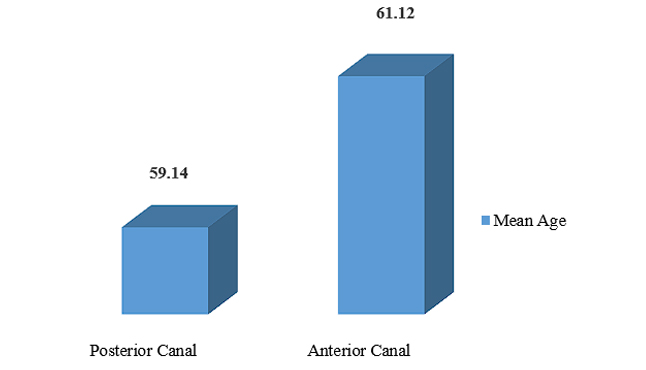
Figure 8. Relationship of Age with the canal involved
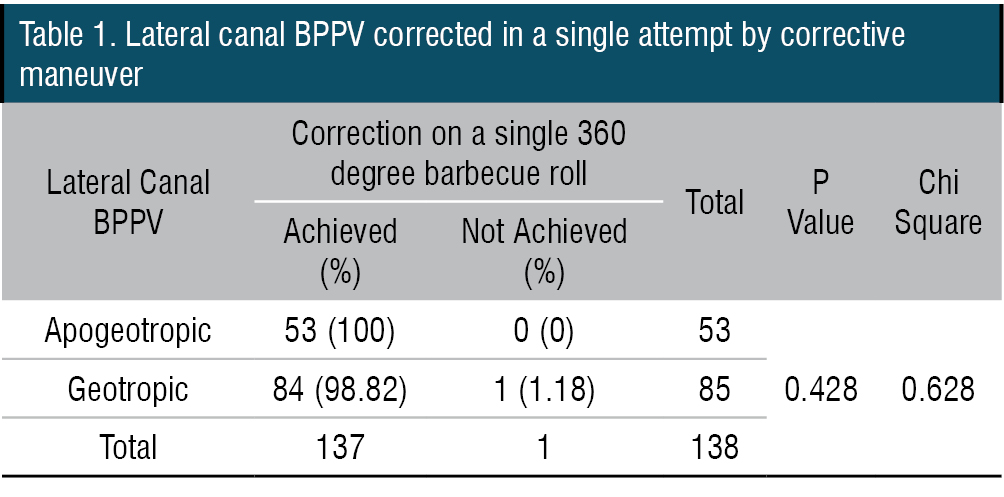
98.82 % of those with geotropic lateral canal BPPV achieved correction at the first time whilst all those were detected apogeotropic lateral canal BPPV achieved correction on a single attempt. The difference in proportion is not significant with p value 0.428 (Table 1).
Whilst all of them presenting with vertigo involving the anterior canal had a symptomatic resolution on a single maneuver, 97.7% of those with posterior canal involvement had relief on a single attempt. This difference in proportion is not significant with p value > 0.05 (1.00) (Table 2).

Discussion
Vertigo, dizziness, imbalance, and unsteadiness can be due to central cause, peripheral cause, loss of physical strength, Increased anxiety, depression, functional cause, cardiovascular cause, and a combination of many. Hence detailed step-wise evaluation is needed for proper diagnosis and management. Vertigo clinics act as a common point to evaluate vertigo due to innumerable causes and accurately treat the patient. In needed cases, if the symptoms are not due to vestibular pathology can redirect the patient to a neurologist, cardiologist, physical medicine, and psychiatrist for proper management of the disease.
We studied the patients who were evaluated in the Rajagiri vertigo clinic based on department protocol. The position test performed with Frenzel glass helps to identify posterior canal BPPV, lateral canal BPPV, geotropic or apogeotropic type, and anterior canal BPPV with accuracy. The appropriate correction maneuvers employed correct the BPPV in most cases with only a few requiring repeat maneuvers. BPPV formed the major cause of peripheral vertigo as per the one-year data from our vertigo clinic.
Vestibular migraine formed the second most common cause of vertigo in our vertigo clinics. Neuhauser and Lempert have given definite and probable criteria for vestibular migraine. Definite vestibular migraine criteria include A. Recurrent vertigo of moderate or severe intensity lasting 5 minutes to 72 hours B. Current or previous history of migraine according to the criteria of the International Classification of Headache Disorders. C. One or more of the following migraine symptoms during at least 50% of the vertigo attacks. Migraine headache, phonophobia, photophobia, aura D. Not attributed to another disorder. Probable vestibular migraine includes A. Recurrent vertigo of moderate or severe intensity lasting 5 minutes to 72 hours B. One of the criteria is B or C for vestibular migraine - migraine history or migraine features during the episode. C. Not attributed to another disorder.1
In our study group, in 83.3% of cases, the history was satisfying the diagnostic criteria. In vestibular migraine patients, normal VNG findings were seen in 28.57% of cases. Abnormal VNG findings were seen in 71.42% of cases. The common abnormalities encountered were saccadic smooth pursuit, gaze-evoked nystagmus, and nystagmus during head positional tests. History not fully satisfying diagnostic criteria with the above-cited abnormal VNG findings was seen in 14.2%. We concluded them as vestibular migraine as they responded to antimigraine therapy. Many patients were not giving an exact history of a headache instead symptoms like the heaviness of the head, inability to tolerate complex visual stimuli, inability to tolerate light, etc. Syncopial migraine and epigone migraine vertigo were two migraine variants encountered during our evaluation.
Vestibular migraine Meniere’s overlap syndrome was more common than pure Meniere’s disease accounting for 3.2% of all cases. Diagnosis of vestibular migraine Meniere’s overlap needed a detailed history. As per the literature When the criteria for Meniere’s disease are met, particularly hearing loss as documented by audiometry, Meniere’s disease should be diagnosed even if migraine symptoms occur during the vestibular attacks. Only patients who have two different types of attacks, one fulfilling the criteria for vestibular migraine and the other for Meniere’s disease should be diagnosed with the two disorders. We expect a future revision of the criteria as vestibular migraine – Meniere’s overlap syndrome, we could see that the majority of our patients were vestibular migraine Meniere’s overlap than pure Meniere’s disease.2
The majority of them had typical symptoms of Meniere’s disease like fluctuant hearing loss, tinnitus, and a longer duration of vertigo in the initial period with established SNHL at the time of presentation. In them, migraine precipitants were triggering the Meniere’s episode. Fluctuant PTA results in the early stages and established hearing loss, in the end, were confirmatory. The heaviness of the head and headaches were associated features. Antimigraine therapy reduced the frequency and severity of Meniere’s episodes in such patients. Abnormal VNG findings seen in migraine were usually seen in vestibular migraine Meniere’s overlap.
The diagnostic criteria for diagnosis of Meniere’s disease are as follows. Definite Meniere’s disease A. Two or more spontaneous episodes of vertigo each lasting 20 minutes to12 hours B. Audiometrically documented low to medium frequency SNHL in one ear on at least one occasion before, during, or after one of the episodes of vertigo C Fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear D. Not better accounted for by another vestibular diagnosis. Probable Meniere’s disease includes two or more episodes of vertigo or dizziness, each lasting 20 minutes to 24 hours B. Fluctuating aural symptoms (hearing, tinnitus, or fullness) in the affected ear D. Not better accounted for by another diagnosis.3
While evaluating patients with meniers in established cases we observed absent caloric on the affected side, features of vestibulopathy in VNG, etc. We managed Meniere’s disease with a lot of reassurance, acetazolamide, and labyrinthine sedatives in the acute stage. Intratympanic gentamycin was employed with success in many cases of Meniere’s disease. Intratympanic dexona was also employed but could see that the benefits of treatment were superior for intratympanic gentamycin therapy than intratympanic dexona.
Patients with acute vertigo during evaluation showing Spontaneous horizontal nystagmus beating towards the healthy side obeying Alexander’s law with pathological head impulse test and absent caloric response on the side affected were diagnosed as vestibular neuronitis. These patients were managed with steroids, and labyrinthine sedatives in the early stages, and vestibular rehabilitation started at the earliest and continued to the late stages. Not all the patients had a typical history of viral prodrome preceding acute vestibular neuronitis. Only 50% had a previous history of viral illness. Hence videonystagmography findings were of use to us in diagnosing vestibular neuronitis in acute-onset vertigo cases. Arguments supporting viral etiology are its endemic occurrence in certain seasons. We could observe that the incidence of vestibular neuronitis was more in certain seasons as per our vertigo clinic records.4
Patients with persistent postural perceptual dizziness (PPPD) had a long duration of dizziness around 3 to 6 months. Some cases had a preceding history of intractable vertigo like BPPV or vestibular migraine, but many had a history of traumatic life events like the loss of a partner, accidents, or untoward events in life preceding chronic dizziness. When evaluated majority of such patients showed normal general examination and VNG findings. They had elevated Hospital Anxiety and Depression Scores.5
They were diagnosed with PPPD and managed with counseling, clinical psychology consultation if needed, and medication.PPPD may be precipitated by peripheral or central vestibular disorder, medical illness, or psychological distress. It is a chronic functional disorder.6
Patients who presented with unsteadiness were assessed by Fullerton score and were suggested vestibular adaptation exercises based on the Fullerton score. We assessed Fullerton’s score before and after treatment.7,8
Vestibular neuronitis and vestibular migraine patient’s Fullerton score improved after treatment. But patients with loss of physical strength needed a longer duration of therapy and we associated with a physical medicine team for rehabilitation of the same.
Many of the patients with recurrent vertigo when evaluated were showing positive central findings in VNG. We Coordinated with the neurology team and they were managed as TIA, stroke, etc according to the diagnosis. As we do a general evaluation before performing VNG we could pick up a central cause even before starting VNG. General detailed evaluation done before videonystagmography is of extreme importance. Patients with progressive supranuclear palsy and parkinsonian-type disorders, lower limb parkinsonism were commonly showing positive retropulsive tests even though not all. Hypsometric saccades, nystagmic intrusions, and slowing of vertical saccades were the central abnormalities commonly encountered. With a detailed history and general examination done before Videonystagmography, we reach a diagnosis in many cases, and videonystagmography with its precision, sensitivity, and objectivity makes the diagnosis. In cases where the cause of recurrent vertigo turned out to be due to cardiogenic stroke, we realized the importance of teamwork and inter-department coordination in diagnosing and treating vertigo cases.
Some Patients with recurrent falls when evaluated the cause turned out to be due to Normal Pressure hydrocephalus, progressive supranuclear palsy. Many cases of vertigo and fall when evaluated turned out to be due to cardiac causes. Falls due to loss of physical strength were another cause. For us vestibular paroxysmia cases were mostly a diagnosis of exclusion. For one of our patients with frequent falls where we could not categorize him as having any other cause of vertigo, management of vestibular paroxysmia with carbamazepine helped.9
Conclusion
Vertigo can be due to a central cause, peripheral cause, psychogenic cause, loss of physical strength, and due to multiple causes. Vertigo clinics with videonystagmography help in detailed evaluation of the patients, ensure complete evaluation and channelize the patients to various departments for proper management. Videonystagmography has improved the quality of diagnosis and management of BPPV and other causes of vertigo due to its objectivity, sensitivity, ability to record and reproduce the findings, ease to use, patient compatibility, and noninvasive technique. We devised a department Protocol at Rajagiri Hospital for ease of management of patients with vertigo. Vertigo clinics with Videonystagmography devised with the proper departmental protocol will improve the diagnosis and management of vertigo.
End Note
Author Information
- Dr Rajesh Raju George, MS ENT
Head of the Department of ENT, Rajagiri Hospital - Dr Dhanya.E.K., DLO, DNB ENT
Senior Consultant, Department of ENT, Rajagiri Hospital - Ms. Abhin Lazer, MSLP
Chief Audiologist, Department of ENT, Rajagiri Hospital - Ms. Swetha, BSLP
Audiologist, Department of ENT, Rajagiri Hospital - Ms. Ahana, MSLP
Audiologist, Department of ENT, Rajagiri Hospital
Acknowledgment:
Dr. Sreenivas Dorasala, Senior Consultant and Co-founder of Cyclops Medtech.
Mr. Brijil, Information Technology, Rajagiri, Hospital.
Dr Susan George Consultant Epidemiologist.
Mr Kevin, AVP Telemedicine.
Financial Support: Nil
Ethical Standards: Matched
Conflict of Interest: None declared
References
- Michael Von Brevern, Chapter 21 Migraine and Other episodic Vestibular disorders, Page 244 - 250.Oxford Textbook of Vertigo and Imbalance Edited by Adolfo M Bronstein.Series Editor Christopher Kennard.
- Lempert, Thomas, Jes Olesen, Joseph Furman, John Waterston, Barry Seemungal, John Carey, Alexander Bisdorff, Maurizio Versino, Stefan Evers, and David Newman-Toker. “Vestibular Migraine: Diagnostic Criteria.” Journal of Vestibular Research 22, no. 4 (January 1, 2012): 167–72.
[Crossref] - Lopez-Escamez, Jose A., John Carey, Won-Ho Chung, Joel A. Goebel, Måns Magnusson, Marco Mandalà, David E. Newman-Toker, et al. “Diagnostic Criteria for Menière’s Disease.” Journal of Vestibular Research: Equilibrium & Orientation 25, no. 1 (2015): 1–7.
[Pubmed] | [Crossref] - Thomas Brandt, Marianne Dieterich Michael Strupp Chapter 2, 2.2 Vestibular Neuritis (Acute Partial Unilateral Vestibular Deficit), page 55- 59. Vertigo and Dizziness Common complaints, Springer.
[Source] - Snaith, R. Philip. “The Hospital Anxiety And Depression Scale.” Health and Quality of Life Outcomes 1 (August 1, 2003): 29.
[Pubmed] | [Crossref] - Staab, Jeffrey P., Annegret Eckhardt-Henn, Arata Horii, Rolf Jacob, Michael Strupp, Thomas Brandt, and Adolfo Bronstein. “Diagnostic Criteria for Persistent Postural-Perceptual Dizziness (PPPD): Consensus Document of the Committee for the Classification of Vestibular Disorders of the Bárány Society.” Journal of Vestibular Research: Equilibrium & Orientation 27, no. 4 (2017): 191–208.
[Pubmed] | [Crossref] - International Journal of Multidisciplinary Educational Research,ISSN:2277-7881; IMPACT FACTOR:7.816(2021);ICVALUE:5.16;ISI VALUE:2.286
- Sakina Katerawala, Khushboo Shah To check Inter-Rater and Intra- Rater Reliability of Fullerton Advanced Balance (FAB)Scale in Stroke patients, International Journal of Health Sciences and Research Vol.10; Issue5;May 2020 Web site: www,ijhr.org ISSN:2249-9571
[Source] - Strupp, Michael, Jose A. Lopez-Escamez, Ji-Soo Kim, Dominik Straumann, Joanna C. Jen, John Carey, Alexandre Bisdorff, and Thomas Brandt. “Vestibular Paroxysmia: Diagnostic Criteria.” Journal of Vestibular Research: Equilibrium & Orientation 26, no. 5–6 (2016): 409–15.
[Pubmed] | [Crossref]