Case Report Published on June 28, 2023
Necrotising Fasciitis Complicating Rhino Orbito
Cerebral Mucormycosis – A Case Report
Prasobh Stalin1
1. Consultant and HOD, Little Flower Hospital and Research Center, Angamaly*
ABSTRACT
Introduction: Mucormycosis became a common life-threatening fungal infection during COVID 19 delta variant wave in India. They have an intrinsic ability to invade blood vessels. Rhino-orbito-cerebral mucormycosis is the most common, and the most aggressive, form of mucormycosis. Uncontrolled metabolic conditions (especially diabetes mellitus in ketoacidosis) is the main risk factor and the core determinant of the world-wide incidence of mucormycosis. Mortality remains high (30-70%) despite advances in diagnosis and treatment
Clinical Discussion: This is the first case of monomicrobial necrotising fasciitis by Pseudomonas secondary to Rhino orbito cerebral mucormycosis. Treatment experience is shared in the article.
Keywords: Necrotising Fasciitis, Pseudomonas Aeruginosa
Case presentation
2.1 History : The subject of interest in this report is a 52 year old lady who had contracted the disease in the very early phase of outbreak and hence her symptoms did not alert her treating physician. It took almost 10 days to be diagnosed as Covid associated mucormycosis after onset of first warning symptoms. Once diagnosed, she got admitted in a nearby primary care hospital where only minimal debridement was done but this centre didn’t have facility for starting liposomal amphotericin B. Hence she was moved to a different centre where liposomal amphotericin B was given for almost a month long period.
Unfortunately, the disease clearance was inadequate hence the drug couldn’t prevent the spread of mucormycosis into her eye and meninges. By this time the metabolic imbalances had made her bedridden. She defaulted on her IV Liposomal Amphotericin B and the mucor by this time made her right eye blind and caused right cavernous sinus thrombosis. It was at this juncture she was shifted to my centre looking for a curative treatment.
Clinical presentation
On right side, facial swelling, eyelid ptosis, chemosis, blind eye were noticeable (Figure 1). Other findings included necrotic black areas on right hard palate and loss of right eyelid elevation.

Figure 1. Clinical presentation - Right facial swelling, Ptosis, Chemosis
She also had headache and fever, severe anemia, hypothyroidism, uncontrolled T2DM and electrolyte imbalances on admission.
Management
As a protocol, we compare MRI contrast image with Fat suppressed T2W image. This helps to identify the necrotic areas within a specified area. It is understood that the area enhancing with contrast is highly inflamed but at the same time, it implies that the area is vascular and hence the antifungal drug Liposomal Amp B can reach the site by intravenous injection. An area which is bright on fat suppressed T2 and having loss of contrast enhancement suggests necrosis at the particular site which needs to be debrided radically to save the patient.
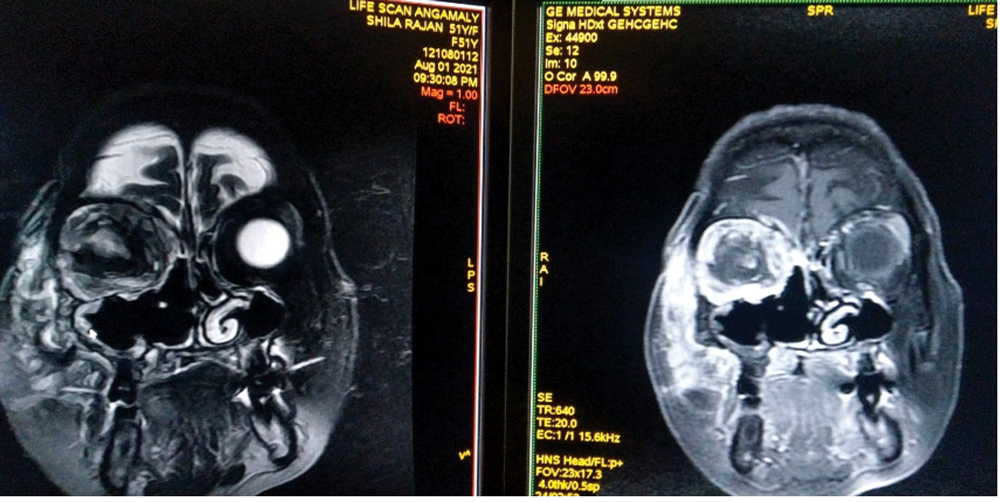
Figure 2. Note bright area on fat suppressed T2 in the centre of right orbit is not enhancing on contrast whereas ocular adnexa seems to be enhancing. Also note the previous surgical changes to maxillary sinus on right.
On all following images, fat suppressed T2W images are given on left and contrast images on right (Figure 2).
As evident from clinical evaluation and imaging, on right side, maxilla, zygoma, pterygoid plates, greater wing of sphenoid, orbital contents and bony segments of orbit adjoining frontal bone were involved. Skin over face was not infiltrated hence could be used to cover the surgical site.

Figure 3. Peroperative finding
Approach started with a right Weber – Fergusson incision and extended laterally over right temporal region to drain a subcutaneous pus collection at this site. Note necrosed maxilla and dehiscence at some areas (Figure 3).
The decision for orbital exenteration was made due to involvement of eyeball in certain sequences and need to remove sequestra in orbital plates
After orbital exenteration and maxillectomy, pterygoid plates were removed. Dehiscence can be noted in superior sutural attachments of orbital bone and were partially removed fearing loss of support to brain and dura.

Figure 4. Primary closure
Primary closure of Weber Fergusson incision with a bolster support was done (Figure 4). She was started on Liposomal Amphotericin B same day. The surgical site also had secondary infection with multidrug resistant pseudomonas due to long standing necrosis in mucor affected areas. She was hence started on IV Piperacillin Tazobactam and Metronidazole.
Follow up and complications encountered: By POD 4, edges of skin at medial canthus started giving way and showed greenish purulent discharge. Now cultures showed Klebsiella and MDR Pseudomonas infection, drug regimen was changed to IV Amikacin and IV Colistin 6m.u which had sensitivity to both organisms. After 1 week of IV Colistin, it was stopped to avoid nephrotoxicity as patient was on Amp–B too. Ciprofloxacin was started as culture showed some sensitivity

Figure 5. Postoperative followup – 3 weeks
Unfortunately, repeated cultures showed Pseudomonas gaining resistance on ongoing IV antibiotics though Klebsiella disappeared from the field. Clinically, necrosis of edges along lateral nasal wall were progressing. By around 3 weeks post op, half of skin cover over orbit necrosed (Figure 5).

Figure 6. Defect closure with temporalis pedicled muscle flap – 4 weeks
Temporalis pedicled muscle flap was used to close defect at 4 weeks post op (Figure 6). This was after giving Ciprofloxacin for 10 days, when cultures started showing minimal growth of pseudomonas. IV Colistin was restarted.

Figure 7. Necrotising fasciitis
Despite being a pedicled flap, it also gave away partially at the lateral nasal margin within 4 days (Figure 7). At the end of around 7 weeks from first surgery, we can see that even a muscle bulk is eaten away by Pseudomonas
Flap advancement and repeated bolster sutures to prevent gaping too met with failure until third attempt when tissue showed some signs of healing.
By the end of 3 months, a meningoencephalocele has started to pop out through the dehiscences in the bony orbit and frontal bone. This could be easily tackled as access to the area was wide open. She recovered swiftly post operatively from this.

Figure 8. Reconstruction with maxillary prosthesis and artificial eye.
Following reconstruction with a maxillary prosthesis and an artificial eye, we could put smile back on her face (Figure 8).
Discussion
The importance of discussion lies in understanding how one should suscpect necrotizing fasciitis in the setting of mucormycosis.
Necrotising fascitis is a subset of the aggressive skin and soft tissue infections (SSTIs) that cause necrosis of the muscle fascia and subcutaneous tissues. This infection typically travels along the fascial plane, which has a poor blood supply, leaving the overlying tissues initially unaffected, potentially delaying diagnosis and surgical intervention. The infectious process can rapidly spread causing infection of the fascia, peri-fascial planes, and cause a secondary infection of the overlying and underlying skin, soft tissue, and muscle.1 Swartz described two types of necrotising fasciitis-Type I where one anaerobic species bacteriods spp and peptostreptococcus is isolated in combination with one or more facultative anaerobic species such as streptococci other than group A and members of enterobacteriaecea eg:escherischia coli, enterobacter, klebklebsiella, proteus. Type II : group A streptococcus is the main pathogen alone or with staphylococcus aureus.2
Mucorales are present in soil and decaying matter, in immunocompetent people, the spores of Mucorales that reach the respiratory tract adhere to the nasal mucus and are eliminated either by swallowing or sneezing, if there is any wound in the mucous membranes, the polymorphonuclear neutrophils phagocytose and destroy the fungal structures. Neutrophils are the host defense against these infections; therefore, individuals with neutropenia or neutrophil dysfunction are at the highest risk. This is seen clinically in leukemia patients and bone marrow transplant patients, who are at the highest risk. Rhizopus arrhizus studies have demonstrated that the ketone bodies present in these patients are metabolized by a ketone reductase, which allows them to survive in conditions with an acid medium; thus, the fungi become hyphal forms in host tissues and then invade blood vessels. This extensive angioinvasion results in vessel thrombosis and tissue necrosis.3
Since both can present similarly or one may precipitate the onset of other, we should deeply investigate to identify and differentiate between fungal and bacterial cause of the disease. After adequate debridement, IV Liposomal Amphotericin B is indicated for Mucormycosis whereas antibiotic therapy is vital to manage necrotising fasciitis.
First case of pseudomanal aeurogenosa necrotising fasciitis was reported in a renal transplant patient in 1998.4 Maqbool et al described a case of necrotising fasciitis involving head and neck where pseudomonas sp was isolated from wound discharge following debridement probably reflecting post operative wound colonisation.5 P.aeuroginosa is usually considered as an opportunistic pathogen which is seldom able to cause severe infections in normal hosts. Necrotising fasciitis caused by pseudomonas aeruginosa is extremely rare. Only four cases were reported in the literature till 2001.6 By 2012 Monomicrobial Necrotising fasciitis by Pseudomonas aeurogenosa were reported in 37 cases out of which those involving face other than occcular adnexa were only two.7 In 2021, there was a case report of concurrent periorbital necrotising faciitis and endophthalmitis.8 After extensive review it was found that there were no cases of monomicrobial pseudomonal necrotising fasciitis reported where underlying cause is ROCM.
Conclusion
- Monomicrobial Necrotising fasciitis by Pseudomonas secondary to Rhino orbito cerebral mucormycosis is little known entity in medical literature.
- Empirical anti-pseudomonal antibiotic is hence warranted in such cases until microbiological and histopathological reports become available.
- Radical debridement is warranted to save life of the patient.
- Hyperbaric oxygen, IVIG, vacuum wound healing techniques and G-CSF (neutropenia) can be tried in the event of impending failure of routine management.
End Note
Author Information
- Dr. Prasobh Stalin, MS ENT,
Consultant and HOD, Little Flower Hospital
and Research Center, Angamaly
Conflict of Interest: None declared.
References
- Leitner C, Hoffmann J, Zerfowski M, Reinert S. Mucormycosis: necrotizing soft tissue lesion of the face1. Journal of oral and maxillofacial surgery. 2003 Nov 1;61(11):1354-8.
[Pubmed] | [Crossref] - Swartz MN. Cellulitis and subcutaneous tissue infections. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 2000:1037-57.
- Hernández JL, Buckley CJ. Mucormycosis. 2019
- Tsekouras AA, Johnson A, Miller G, Orton HI. Pseudomonas aeruginosa necrotizing fasciitis: a case report. J Infect. 1998 Sep;37(2):188–90.
[Pubmed] | [Crossref] - Maqbool M, Ahmad R, Ahmed R, Qazi S. Necrotising fasciitis in the head and neck region. Br J Plast Surg. 1992;45(6):481–3.
[Pubmed] | [Crossref] - Jaing TH, Huang CS, Chiu CH, Huang YC, Kong MS, Liu WM. Surgical implications of pseudomonas aeruginosa necrotizing fasciitis in a child with acute lymphoblastic leukemia. J Pediatr Surg. 2001 Jun;36(6):948–50.
[Pubmed] | [Crossref] - Reisman J, Weinberg A, Ponte C, Kradin R. Monomicrobial Pseudomonas necrotizing fasciitis: A case of infection by two strains and a review of 37 cases in the literature. Scandinavian journal of infectious diseases. 2011 Nov 29;44:216–21.
[Crossref] - Lee YK, Lai CC. Concurrent Pseudomonas Periorbital Necrotizing Fasciitis and Endophthalmitis: A Case Report and Literature Review. Pathogens. 2021 Jul 7;10(7):854.
[Pubmed] | [Crossref]