Case Report Published on June 28, 2023
Diffuse Large B Cell Lymphoma Mimicking Ulceroproliferative Lesion
Anila Melody Thomas1, J Kiranjith1, Krishnan K1
1. Department of ENT, Sree Gokulam Medical College and Hospital, Venjarammoodu, Kerala*
ABSTRACT
Introduction: Oropharynx contains abundance of lymphoid tissue, particularly in the palatine and lingual tonsils which forms the anterolateral components of Waldeyers ring. Lymphomas arising in the oropharynx are almost exclusively Non Hodgkins lymphoma and arise in lymphoid tissue.
Methods: A case of 69 year old male with Non Hodgkins Lymphoma. Oropharynx, discussing clinical features, radiological and histopathological findings and management.
Discussion: Majority of the patients with Non Hodgkins Lymphoma presents with neck swellings, even though infections and inflammatory conditions can also lead to lymphadenopathy, with available modalities of investigations along with clinical examination, early diagnosis and treatment can be helpful to save life.
Results: A case of diffuse large B Cell Lymphoma with presenting complaints of neck swelling, odynophagia and dysphagia, mimicking oropharyngeal squamous cell carcinoma on clinical examination. Biopsy taken from the lesion showed diffuse large B Cell lymphoma. Patient was started on chemotherapy, but was unable to save life due to poor prognosis.
Conclusion: Non Hodgkins Lymphoma of Oropharynx can mimic Squamous Cell Carcinoma. Better patient awareness and early detection might have reduced the mortality. DLBCL has a poor prognosis.
Keywords: Non Hodgkins Lymphoma, Diffuse Large B Cell Lymphoma
INTRODUCTION
Oropharynx contains abundance of lymphoid tissue, particularly in the palatine and lingual tonsils which forms the anterolateral components of Waldeyers ring. Lymphomas arising in the oropharynx are almost exclusively Non Hodgkins lymphoma and arise in lymphoid tissue.
They present in younger patients (45-55 yrs), diagnosed by biopsy and thereafter treated by haematooncologists.
CASE PRESENTATION
69 old Male presented with complaints of swelling of 5 x 5cms over left side of neck of 1 month duration, which was gradually progressing in size, associated with occasional pain. He also complained of dysphagia & odynophagia since 10 days. There was history of foreign body sensation of throat and change in voice since 6 days. History of snoring & halitosis was present. He also had left ear pain. Bilateral level 1b and Left level V lymphnodes were palpable. On Oral cavity examination, An ulcer proliferative lesion involving base of tongue on left side extending laterally to the left tonsillar fossa and anterior pillar, continuing into the soft palate. Medially it was just crossing the midline. It was hard in consistency with induration, non tender, slough was present over it. It didn’t bleed on touch (Figure 1)
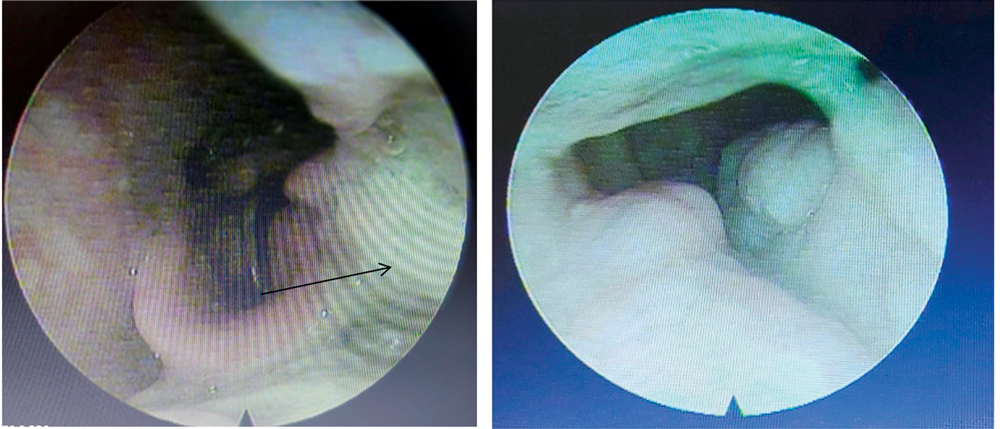
Figure 1 (a &b). Oral Cavity Examination (a), Confirmed by Videolaryngoscopy (b)
CECT Neck Axial cut showed heterogenously enhancing lesion occupying left parapharyngeal space, medially pushing the airway and laterally reaching till parotid and posteriorly till retropharyngeal space. Anteriorly it extended till retromolar trigone, involving left vallecula and inferiorly it reaches just below hyoid bone (Figure 2)
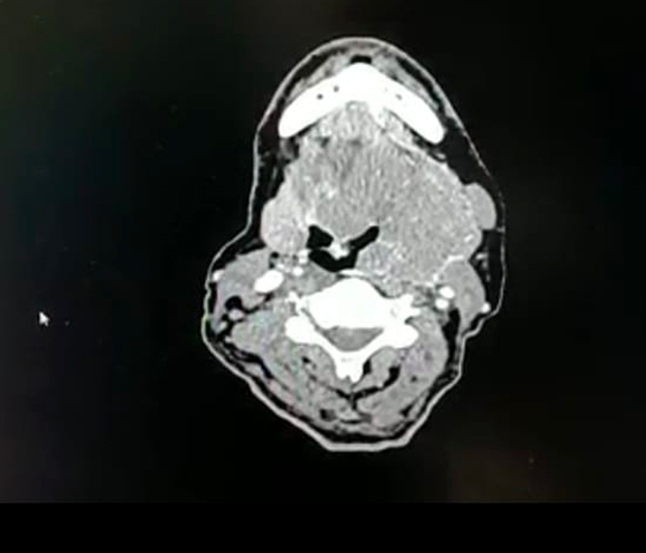
Figure 2. CECT Neck Axial Cut showing lesion occupying Parapharyngeal Space
Peripheral smear showed Neutrophilic leucocytosis with relative eosinophilia.
FNAC from Left submandibular lymph node showed reactive lymphadenitis, negative for atypical or malignant cells.
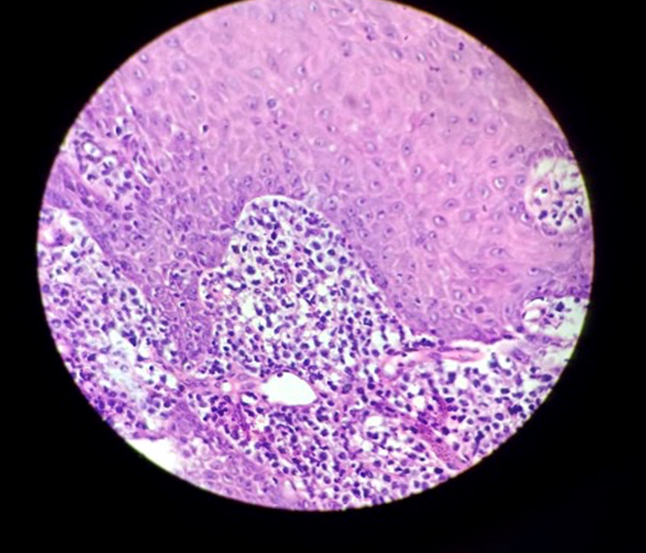
Figure 3. Biopsy from the lesion showing large cells with moderate to clear eosinophilic cytoplasm and enlarged pleomorphic vesicular nuclei with prominent nucleoli. Mitosis 3-4/HPF.
Necrosis present. Overlying epithelium was hyperplastic.
Punch biopsy taken from base of tongue revealed lymphoid tissue lined by stratified squamous epithelium with underlying neoplasm composed of diffuse sheets of atypical lymphoid cells (Figure 3).
So was Started on chemotherapy with R -CHOP regimen, after immunohistochemistry confirmation, but unfortunately couldn’t save the patient.
DISCUSSION
NHL is a group of neoplasms with lymphoreticular systems origin.
Corresponds to 0.2-2% of all the lymphomas. More common in males than females. Extranodal site of occurrence corresponds to 40%. Only less than 1% of all head and neck cancers. Occurance more in Tonsil > Nasopharynx > Base of tongue.
Risk factors include Immunodeficiency, EBV, Autoimmune disease, Hepatitis C, H-pylori infection. Prognostic factors In addition to the REAL classification, a robust prognostic scoring system has been developed. It has long been appreciated that within the same lymphoma subtype there are factors which help predict patients with a poor outcome, for example the presence of ‘B’ symptoms (weight loss, night sweats and fevers). The International Prognostic Index (IPI) divides patients into four specific risk groups at diagnosis: high, high-intermediate, low-intermediate and low. The factors which make up the index are: age, performance status, stage of disease, number of extranodal sites of disease, serum lactate dehydrogenase.1
Diagnosis
The majority of patients present with painless lymphadenopathy. Although infections and inflammatory conditions can lead to lymphadenopathy, persistently enlarged nodes require surgical excision. Fine needle aspiration is not adequate if lymphoma is suspected, for several reasons: Tumour cells do not always uniformly invade lymph nodes, so normal cytology does not exclude disease. Reactive and malignant lymphocytes can be morphologically similar. It is increasingly important to subclassify NHL, for which fresh intact nodal tissue is ideal. Lymphomas may present in many other ways to the general physician, with an increasing number presenting in extranodal sites such as the gastrointestinal tract.
Many lymphoma subtypes are associated with specific cytogenetic abnormalities. For example: (14;18) in follicular NHL (8;14) in Burkitt’s NHL (11;14) in mantle cell NHL2
With increasing application of molecular testing, particularly poly-merase chain reaction, and more recently fluorescence in situ hybridisation, it has become relatively easy to detect these translocations. This can be helpful to differentiate between reactive and malignant lymph nodes where the histology is inconclusive, but it can also be applied following therapy to detect evidence of minimal residual disease. The newly evolving technique of microarray analysis, with which multiple known translocations can be looked for simultaneously, may in future not only be used for NHL diagnosis but may lead to reclassification based on molecular abnormalities rather than on histological features.3
Treatment
Initial treatment has changed little over the last three decades for the majority of patients with NHL. Where disease is localised, radiotherapy is often employed irrespective of disease type. For aggressive lymphomas, the drug combination cyclophosphamide, doxorubicin, vincristine and prednisolone (CHOP) remains the gold standard. A number of five- and six-agent regimens briefly appeared superior, but this was not confirmed in large phase III studies.5 Following relapse, salvage HDT, consolidated by an autologous transplant, is evidence-based standard therapy, but applicable only to younger patients. Treatment in indolent lymphoma is effectively palliative but, with median survivals of ten years in the commonest subtypes, the fact that the disease is not ‘curable’ may be irrelevant. Many drugs will induce remissions for these lymphomas. Increasingly, purine analogue drugs, particularly fludarabine, are being used in the indolent lymphomas, usually in the relapsed setting and often in combination with other chemotherapeutic agents. Purine analogues lead to a profound lymphocytopenia, which can last for many months post-therapy and predisposes these patients to opportunistic infections, thus making Pneumocystis carinii pneumonia prophylaxis essential.4
New approaches
Two potential advances in the management of NHL are becoming established in clinical practice. Monoclonal antibody therapy Lymphoma provides a good target for monoclonal antibody therapy as the malignant cells have abundant membrane-bound antigens confined to the tumour and renewable tissue. Antibodies against CD20, a membrane bound antigen found on many forms of B cell lymphoma, have been developed and are now licensed. This antibody binds to the cell surface and kills tumour cells through a number of mechanisms including cell-mediated and complement-mediated cytotoxicity and the induction of apoptosis. Treatment is given by weekly infusion, and is generally well tolerated although immediate hypersensitivity reactions can occur. However, it does not have the side effects commonly associated with chemotherapy, namely hair loss, nausea, vomiting and suppression of the bone marrow. Response rates of up to 60%have been seen in follicular lymphomas when used as a single agent, but the exciting prospect is its combination with standard chemotherapy where response rates appear significantly better than with chemotherapy alone . In newer agents the anti-CD20 antibody is conjugated with a radioactive moiety which effectively delivers local radiotherapy directly into the tumour, often with impressive clinical result.5
Bone marrow (stem cell) transplantation
The other evolving field is bone marrow (stem cell) transplantation. Autologous transplantation is established in the management of relapsed aggressive NHL, and also in selected younger patients with more indolent diseases.
CONCLUSION
As with all forms of cancer, it is important for patients with NHL to be referred to the appropriate local clinic. Patients should be offered a multidisciplinary approach to both diagnosis and therapy. The latter may require a combination of treatments including chemotherapy, radiotherapy, transplantation and, in future, immune-based therapies.
End Note
Author Information
- Dr. Anila Melody Thomas,
Post Graduate Resident,
Department of ENT, Sree Gokulam Medical College and Hospital, Venjarammoodu, Kerala
- Dr J Kiranjith, Professor, Department of ENT,
Sree Gokulam Medical College and Hospital, Venjarammoodu, Kerala
- Dr Krishnan K, Assistant Professor,
Department of Ent, Sree Gokulam Medical College and Hospital, Venjarammoodu, Kerala
Conflict of Interest: None declared.
REFERENCES
- Flint PW, Haughey BH, Lund VJ, Niparko JK, Robbins KT, Thomas JR, et al. Cummings Otolaryngology - Head and Neck Surgery E-Book. 6th edition. Saunders; 2014. 16273 p.
[Source] - Robbins cotran pathological basis of disease- 8 th edition pg no 145 to 170,chapter Neoplasia
- Scottbrown- 8 th edition,volume 3,pg no-207 to 237,chapter oropharyngeal malignancies,Barnes L,Eveson J W,Reichart P
- Liu C, Delaney S, Brown TN. An Unusual Presentation of B-Cell Lymphoma as a Large Isolated Epiglottic Mass: Case Report and Literature Review. Case Rep Otolaryngol. 2016;2016:9787432.
[Crossref] | [Pubmed] - Rule S. Non-Hodgkin’s lymphoma. Clin Med (Lond). 2001;1(5):362–4.
[Pubmed] | [Crossref]