Case Report Published on June 28, 2023
Olfactory Groove Meningioma –A Case Report
Vivek Sasindran1, Rashmida E M2
1. Department of Otorhinolaryngology, Pushpagiri Institute of Medical Science and Research Centre, Thiruvalla;
2. PG Resident, Pushpagiri Institute of Medical Science and Research Centre, Thiruvalla*
ABSTRACT
Introduction
- Olfactory groove meningiomas are rare anterior cranial fossa meningiomas, constituting 8 – 13% of all intracranial meningiomas.1
Case Report
- 54/F with SNHL on left side, ipsilateral trigeminal nerve involvement and impaired cerebellar function tests.
- she also had absent smell sensation for last 2-3 years but it was never her primary complaint.
- MRI showed CP angle lesion on left side and surprisingly another lesion in the olfactory groove, suggestive of meningioma.
- Excision of CP angle tumour was done and olfactory groove meningioma was kept on follow up. During follow up, progressive increase in size of the lesion was noted and hence endoscopic trans nasal excision of olfactory groove meningioma was done.
- Postoperative period was uneventful.
Conclusion
- Complete Surgical excision is the definitive treatment of skull base meningioma.
- Endoscopic approach has less morbidity as opposed to the traditional open approaches but proper case selection is the key.
- This case also highlights the importance of evaluating patient with anosmia which might be ignored by the patient.
Keywords: Olfactory Groove Meningioma, Transnasal Endoscopic Approach
Meningiomas are the most common non glial primary brain tumor. Approximately 30 percent of all brain tumors are meningiomas. They can occur in different sites. Olfactory groove meningiomas are rare and it accounts for about 8 -13% of intracranial meningiomas. These arise from the cribriform plate and the frontoethmoidal suture in the anterior cranial fossa.1,2
Olfactory groove meningioma is typically a slow - growing tumour, patients are asymptomatic for a longer period before the diagnosis. At times it can be an incidental finding while evaluating for other pathologies.3
The most common clinical features are headaches and olfactory dysfunction. If it is large it can compress the frontal lobe and optic chiasma to cause personality changes, seizures, and visual disturbances respectively.4-6
If it is asymptomatic and slow growing, wait and watch policy can be adopted. Complete surgical excision remains the definitive treatment of olfactory groove meningioma.7
CASE REPORT
54-year-old female presented with complaints of hearing loss on the left side for 1-year duration, occasional unsteadiness for 2 weeks, and numbness of the left side of the face for 2 weeks. She also had reduced smell sensation for the last 1 year with history of nasal allergy. She was on intranasal steroids. No other nasal complaints, headache, visual disturbances, or personality changes were present.
Examination showed sensory neural hearing loss on the left side, decreased corneal sensitivity, reduced sensation over the left side of the face, and absent smell sensation.
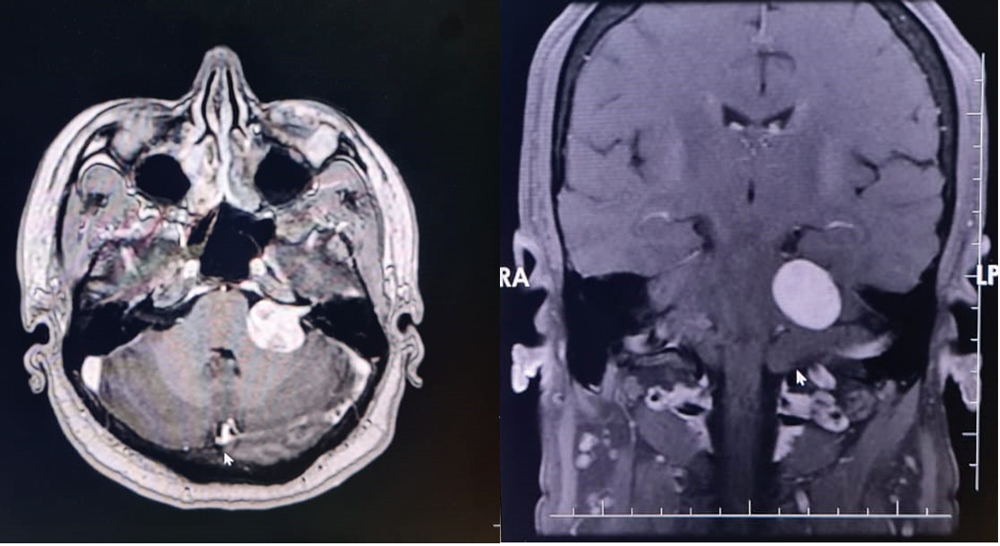
Figure 1. Axial and coronal view of left CP angle lesion with intracanalicular extension
MRI with gadolinium contrast was done which showed a well-defined lobulated heterogeneous intensely enhancing extra-axial lesion in the left CP angle with intracanalicular extension which was suggestive of Acoustic schwannoma (Figure 1)
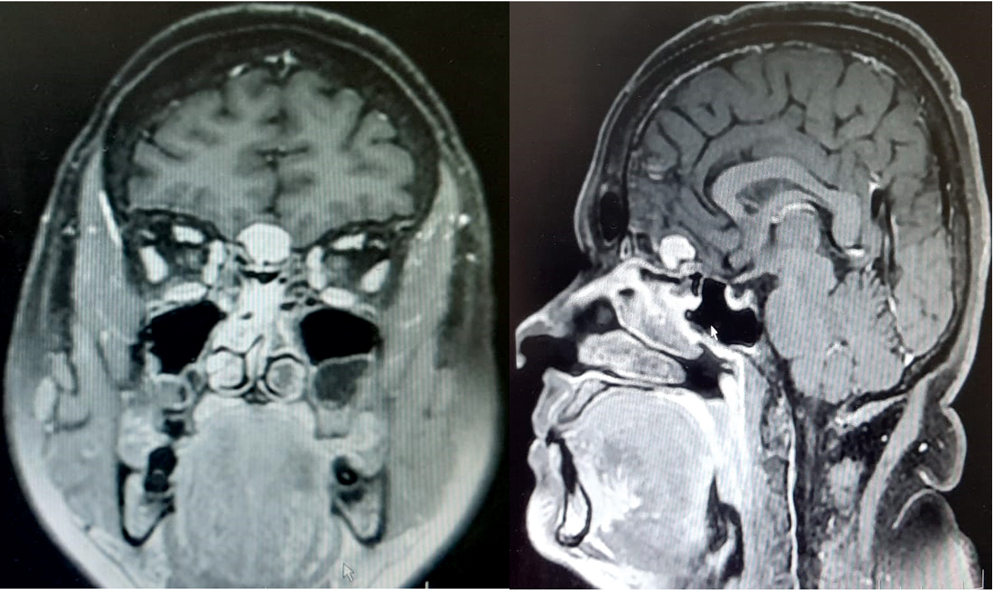
Figure 2. Lesion in the olfactory fossa
Another well-defined lobulated homogenously enhancing lesion was identified in the anterior cranial fossa with “dural tail sign” filling the olfactory fossa, possibly olfactory groove meningioma (Figure 2).
The CP angle tumour was taken up for excision via extended retrosigmoid approach and the anterior cranial fossa lesion was kept on follow-up. In the subsequent MRI, the size of the anterior cranial fossa lesion was found to be increasing, and hence 3 months later Endoscopic transnasal excision - Binostril four-handed technique was planned.
OPERATIVE PROCEDURE
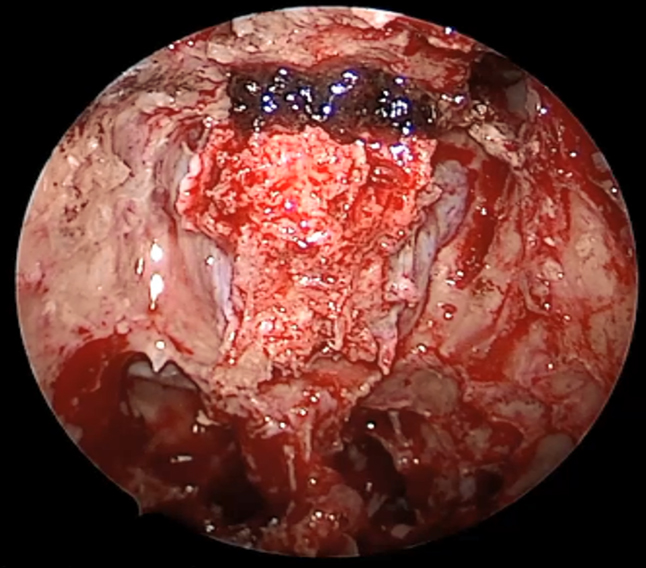
Figure 3. After completion of osteotomy on all sides.
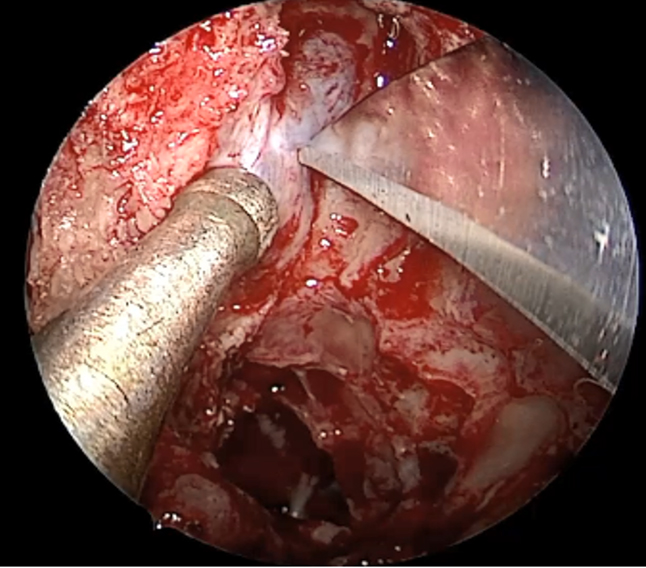
Figure 4. Dural incision on left side
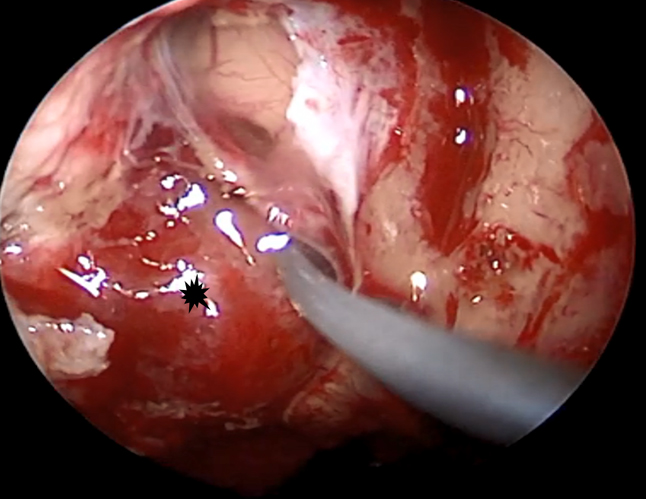
Figure 5. Dissection of tumour from arachnoid
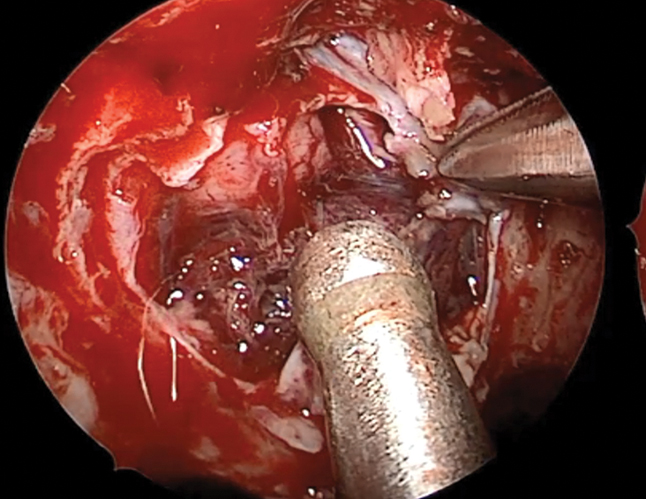
Figure 6. Delivering the tumour from brain parenchyma
Bilateral frontoethmoidosphenoidotomy was done, nasoseptal flap was harvested, posterior superior septal window was created to facilitate binostril four handed technique. Fovea ethmoidalis and lateral lamella of cribriform was delineated on either sides. Anterior and posterior ethmoid arteries were cauterised. Osteotomy was performed in the roof of ethmoid on either sides, anterior cut was made anterior to the cribriform and posterior cuts posterior to the cribriform plate, bone was removed (Figure 3). Dural incision was placed and extended on left side (Figure 4). Olfactory bulb was identified, the tumour was identified and dissected from arachnoid and the brain parenchyma and sent for histopathology (Figure 8, 9). After ensuring the complete removal, reconstruction was done (Figure 5-9).
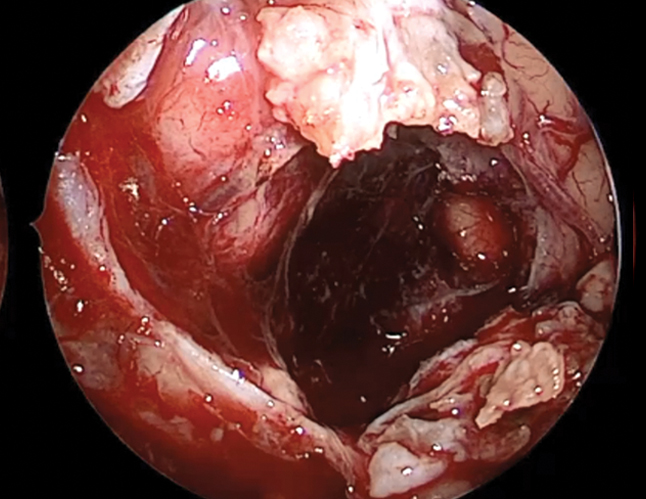
Figure 7. After complete removal of the tumour
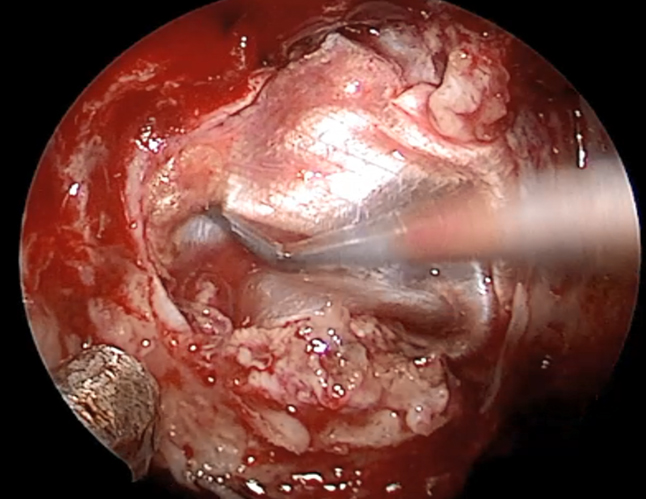
Figure 8. Inlay layer of facia lata
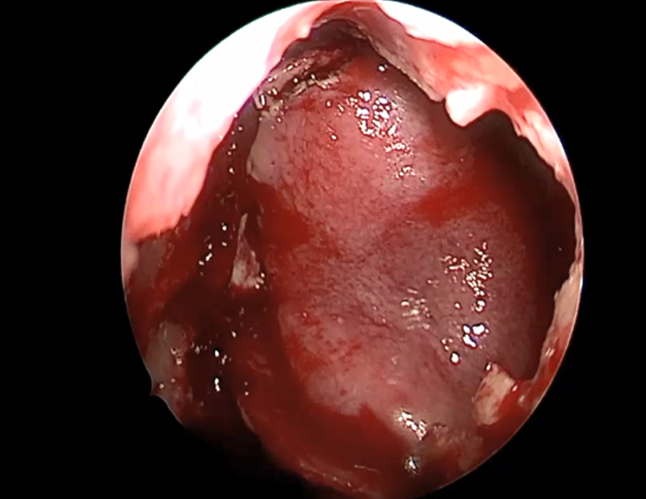
Figure 9. Nasoseptal flap
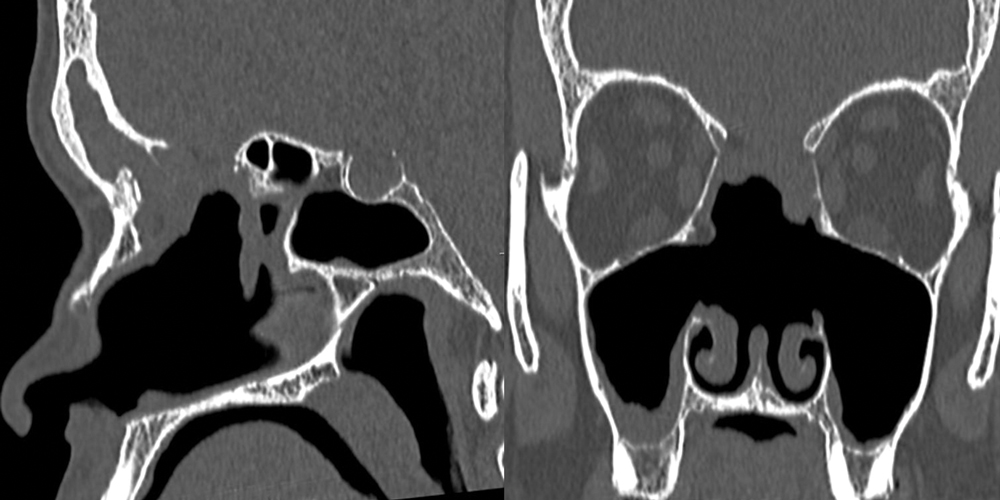
Figure 10. Postoperative CT scan – reconstructed flap in position
DISCUSSION
Olfactory groove meningioma originates from the arachnoidal cells which are embedded in the midline dural covering of the cribriform plate and frontosphenoidal suture. The microscopic appearance, pathologic classification, female preponderance are like meningiomas found elsewhere.3
WHO CLASSIFICATION of meningioma is Grade 1 – Typical, Grade 2 – Atypical, Grade 3 – Anaplastic – with a high recurrence rate.
Hyposmia /anosmia is usually the early presentation; headache is often associated with it. As the lesion enlarges it causes compression of the nearby structures and presents with varying features, compression of optic nerve fibres and optic chiasma leading to visual disturbances, if it is very large it can compress the frontal lobe of the brain, causing behavioural changes and siezures. It can also be an incidental finding when imaging is done for other pathologies as with this case.7
MRI with and without gadolinium enhancement is the imaging of choice which classically shows a lesion in the olfactory groove which is isointense on T1 and T2 weighted images with “Dural tail sign”. CT scan with fine cuts through the anterior skull base is also necessary prior to the surgical excision. It also helps to make out the extension into the paranasal sinuses.3
The differential diagnosis are Olfactory nerve schwannoma which is rare, it could be differentiated from imaging. Bony sclerosis and the dural tail is absent with respect to olfactory groove meningioma. Esthesioneuroblastomas, Dural-based metastases, and Tuberculum sellae meningiomas are the other differential diagnosis.
Ideal management of skull base meningioma is surgery. There are different approaches like Bifrontal Craniotomy, Transnasal Endoscopic approach. The advantages of bifrontal craniotomy are complete resection of the tumour including dural tail is possible even for large tumours with less risk of CSF leak. If the olfaction is present preoperatively, it might preserve it. Disadvantages are the requirement of large bone openings, risk of brain retraction along with morbidity of a major neurosurgical procedure whereas transnasal endoscopic approach carries less neurovascular complications with no risk of brain retraction, better illumination and excellent surgical access but the disadvantages are increased risk of CSF leak and postoperative infection, permanent loss of smell.
Extent of primary surgery is critical for long term cure rates. Proper patient selection is important. we should consider the vertical height of tumour and the lateral extension, endoscopic access beyond mid pupillary line may be challenging.8
Skull base reconstruction is done after an extended endoscopic approach to establish the segregation of the intracranial structures and the sinonasal cavity. Reconstruction can prevent the postoperative complications, CSF leaks and intracranial infections.
Minor skull base defects can be reconstructed using techniques like placing surgicel, fat, tissue glue etc. However, larger defects and patients with a high risk of CSF leaks like previous radiotherapy, morbidly obese are better treated using vascularized tissue.
The “Hadad-Bassagasteguy flap”, as part of a multilayer technique, is one of the preferred option when reconstructing the skull base if available. This vascular pedicle comprises the posterior septal artery which is the terminal branch of the sphenopalatine artery. This flap is harvested during the initial steps of the surgical approach, and it can be designed according to the size and shape of the defect. The flap is kept in the nasopharynx during the procedure and is retrieved when needed.8
Conservative management can be adopted for very slow growing small asymptomatic patients particularly old age. Radiotherapy and Stereotactic radiosurgery are the other options.
CONCLUSION
Olfactory groove meningioma was diagnosed incidentally in this case when evaluating a CP angle lesion. Anosmia was present but the patient ignored the symptom. The lesion was present in the olfactory groove without much lateral extension and hence this case was an ideal case for transnasal endoscopic excision.
This also highlights the importance of workup of patient with olfactory dysfunction.
Extended endonasal approaches are safe and effective for the treatment of a variety of anterior skull base lesions, requires proper equipment and experience to ensure their efficacy and safety.8
End Note
Author Information
- Dr Vivek Sasindran MBBS, MS ENT
Professor, Otorhinolaryngology
Pushpagiri Institute of Medical Science and Research Centre, Thiruvalla - DR Rashmida E M
PG Resident
Pushpagiri Institute of Medical Science and Research Centre, Thiruvalla
Conflict of Interest: None declared
Acknowledgement: Authors confirm that there is no conflict of interest in this case report.
REFERENCES
- Farooq G, Rehman L, Bokhari I, Rizvi SRH. Modern Microsurgical Resection of Olfactory Groove Meningiomas by Classical Bicoronal Subfrontal Approach without Orbital Osteotomies. Asian J Neurosurg. 2018;13(2):258–63.
[Pubmed] | [Crossref] - Aguiar PHP de, Tahara A, Almeida AN, Simm R, Silva AN da, Maldaun MVC, et al. Olfactory groove meningiomas: approaches and complications. J Clin Neurosci. 2009 Sep;16(9):1168–73.
[Pubmed] | [Crossref] - Ikhuoriah T, Oboh D, Abramowitz C, Musheyev Y, Cohen R. Olfactory groove meningioma: A case report with typical clinical and radiologic features in a 74-year-old Nigerian male. Radiol Case Rep. 2022 Sep 26;17(12):4492–7.
[Pubmed] | [Crossref] - Mejbri M, Karmani N, Ayadi K, Slimene A, Abderrahmen K, Kallel J. Otolaryngology : Open Access Olfactory Groove Meningioma : Clinical Presentation and Surgical Outcomes of Subfrontal Approach , Experience of The National Institute of Neurology of Tunisia. 2020;10(6).
- Colli BO, Carlotti CG, Assirati JA, Santos MBM dos, Neder L, Santos AC dos, et al. Olfactory groove meningiomas: surgical technique and follow-up review. Arq Neuropsiquiatr. 2007 Sep;65(3B):795–9.
[Pubmed] | [Crossref] - Niklassen AS, Jørgensen RL, Fjaeldstad AW. Olfactory groove meningioma with a 10-year history of smell loss and olfactory recovery after surgery. BMJ Case Rep. 2021 Aug 25;14(8):e244145.
[Pubmed] | [Crossref] - Pepper JP, Hecht SL, Gebarski SS, Lin EM, Sullivan SE, Marentette LJ. Olfactory groove meningioma: discussion of clinical presentation and surgical outcomes following excision via the subcranial approach. Laryngoscope. 2011 Nov;121(11):2282–9.
[Pubmed] | [Crossref] - Ditzel Filho LFS, de Lara D, Prevedello DM, Kasemsiri P, Otto BA, Old M, et al. Expanded endonasal approaches to the anterior skull base. Otorhinolaryngol Clin. 2011;3(3):176–83.
[Source]