Original Research Published on June 28, 2023
Long- Term Outcomes in Obstructive Salivary Gland Disease due to Calculus after Sialendoscopy
Bini Faizal1, Ammu Dileep1, Greeshma CR2
1. Department of ENT, Amrita institute of Medical Sciences, Amrita Vishwa Vidyapeedham University, Kochi, India;
2. Lecturer, Department of Biostatistics, Amrita institute of Medical Sciences, Amrita Vishwa Vidyapeedham University, Kochi, India*
ABSTRACT
Background: The introduction of sialendoscopy has brought about a paradigm shift in salivary calculi management.
Objectives: To assess the long-term outcomes of sialendoscopy in obstructive salivary gland disease due to calculi.
Methods: This was a prospective observational study conducted among 65 patients of sialolithiasis who underwent interventional sialendoscopy for the same. Subjective assessments of salivary gland function were done before and after the procedure during pre- operative, and at first, sixth and twelfth month post- operative visits. The assessment was done by Chronic Obstructive Sialadenitis Symptoms(COSS) Questionnaire.
Results: Interventional sialendoscopy for sialolithiasis showed statistically significant improvement in COSS scores during all stages of evaluation.
Conclusions: Long-term evaluation of patients treated by interventional sialendoscopy showed good outcomes for sialolithiasis which were maintained at the end of one year after procedure. The positive outcome stresses the need for salivary gland preservation in sialolithiasis with a need for more centres practising sialendoscopy.
Keywords: Sialendoscopy, Sialolithiasis, Ductal Stenosis, Sialadenitis, Level of Evidence: Level III
INTRODUCTION
Sialendoscopy introduced in 1993 has revolutionised the treatment of benign inflammatory salivary gland disorders.1 Sialadenectomy and related surgical risks can be avoided by this technique along with retaining salivary function. Since it is a new procedure the long-term outcomes of the procedure are not well known.2 There is a chance of development of ductal stenosis several months later during the remodeling phase due to cicatrix. Besides, a salvaged gland may not be functional raising the question of the need to resort to these interventions. Some of the patients may need repeated procedures without satisfactory improvement in symptoms resulting in multiple visits to the hospital and increased cost of health care. Failed cases may finally require sialadenectomy. In a similar situation, knowledge of the limitations of sialendoscopy will help a surgeon decide upon sialadenectomy upfront. Sialendoscopy involves trained surgeons, dedicated technicians for equipment maintenence, additional investment and disposable materials like baskets and stents which are expensive. There are very few centres practising sialendoscopy which furthur limits access to quality health care. With this background, the efficacy and the long-term outcomes of sialendoscopy in terms of functionality and symptoms need to be evaluated. This study was conducted to assess the efficacy and safety of techniques in sialendoscopy practised in this institution for obstructive salivary pathology due to calculus.
MATERIALS AND METHODS
This was a prospective observational study conducted at a tertiary care centre, over a period of two years (September 2020 to August 2022), after approval from the ethical committee (ECASM-AIMS-2021-260). The ethical standards and guidelines in the Declaration of Helsinki were adhered to and informed consent was taken from all patients. The study included 65 patients who underwent sialendoscopy for sialolithiasis.
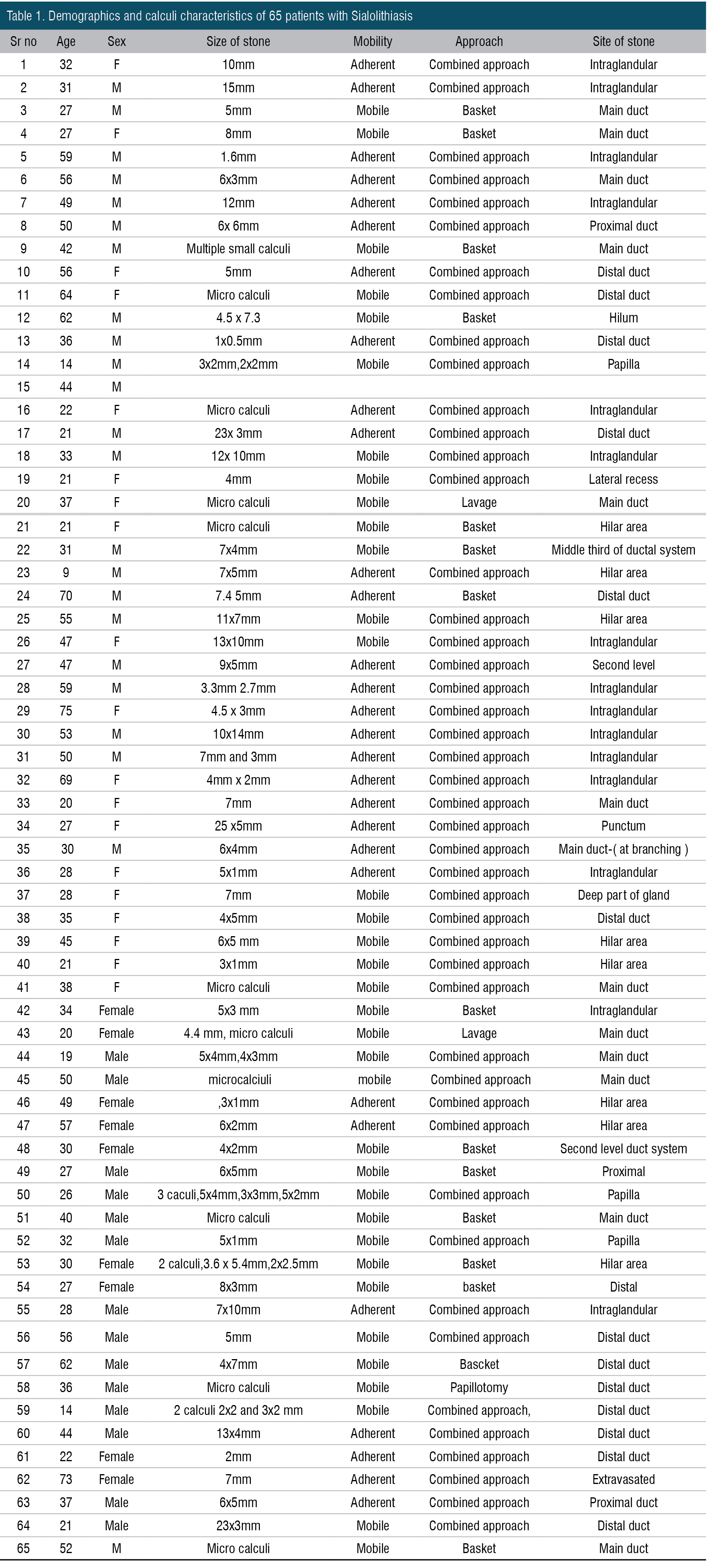
The study was conducted among patients of all age groups coming to the ENT department with the diagnosis of sialolithiasis based on clinical examination, ultrasound and in selected cases, CT scan. All the patients underwent interventional sialendoscopy under general anaesthesia, and were discharged the next day and reviewed at 1 month, six months and one year after the procedure (Table 1). Subjective assessment of salivary gland function was done before and after the procedure at each visit. The assessment was done by COSS questionnaire.3,4 Main symptoms like pain or discomfort, swelling and saliva production were assessed separately. The COSS questionnaire, which analysed 10 gland-specific symptoms that may influence social functioning, as well as 10 general questions about salivary function, oral function, and quality of life, is a patient-reported symptom assessment tool. The patients rated each question on a scale of 0 to 10, and the total scores were recorded in percentage, zero being the best score. Pain or discomfort score was given out of 220 (2 questions carried a score of 10 and 2 questions carried a score of 100; 2x100+2x10=220). The swelling was scored out of 240 ( 6 questions from the COSS questionnaire in which 2 questions carried a score of 100 and 4 questions carried a score of 10;2x 100 +4x 10 =240). The saliva production was scored out of 100 which was also included in the COSS questionnaire. There were 65 patients in the study. At the end of one year, 42 patients were available for evaluation. The remaining 33 patients had completed 6 months of follow-up. There were no dropouts or adverse events reported during the period.
STATISTICAL ANALYSIS
Statistical analysis was done using IBM SPSS 20. (SPSS Inc, Chicago, USA). For all continuous variables, the results were represented as Mean+/-SD, and for categorical variables as frequency and percentage. To compare the Preoperative and postoperative numerical variables, paired t-test was applied. A p-value of 0.05 was considered statistically significant.
RESULTS
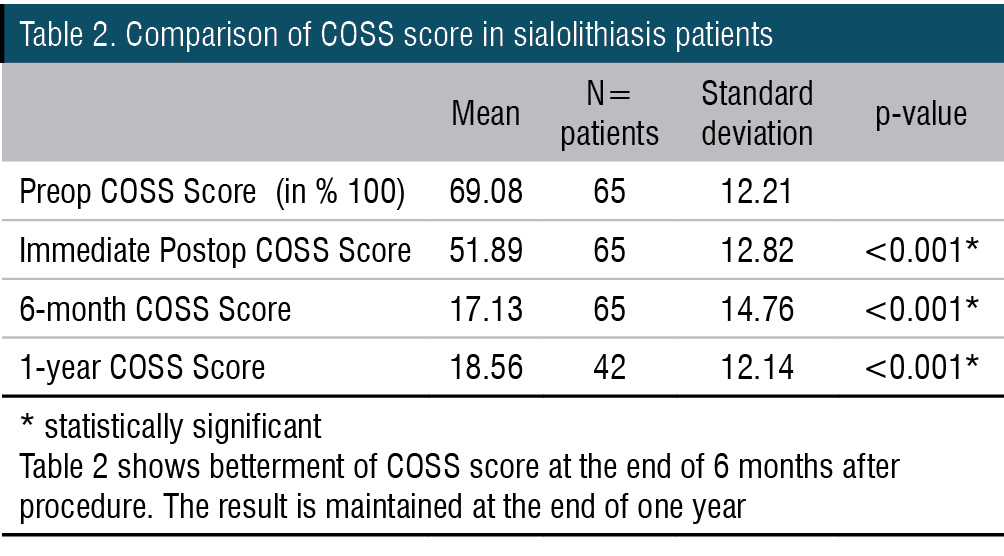
Out of 65 patients with sialolithiasis, the mean COSS scores in the preoperative and postoperaive period were 69.08 +/- 12.21 and 51.89 +/- 12.82 respectively (Table 2). The mean COSS scores were 17.13+/- 14.76 in the 6-month postoperative period which were statistically significant. Forty two patients were available for one year follow-up and the mean COSS scores were 18.56+/-12.14. The comparison of the mean between the pre-operative and 1-year post-operative period was found to be statistically significant (p = <0.001). In the study, the size of stones ranged from micro calculus(1mm) to 23mm.
DISCUSSION
The most common site of salivary stone formation (80%) is the submandibular gland, with 20% occurring in the parotid gland.5,6 Our study which included 65 patients of sialolithiasis showed predominant submandibular gland involvement compared to parotid, being 59(60.8%) and 38(39.2%) respectively. The study by Moorthy et al. showed 52 % submandibular involvement and 48% parotid involvement.7 Out of 65 patients, 12.4% were under 18 years of age. In the study, the imaging modality most commonly used was ultrasonography. CT scan was performed when USG was not contributory in a patient with mealtime syndrome. Whether a stone can be extracted with sialendoscopy alone does not depend solely on its size but also on its shape. It is therefore possible to extract very long, thin stones from the duct with sialendoscopy.8 The size of stones ranged from microcalculus (1mm) to 23mm. Small and mobile calculus was removed using Cook’s 4 wire tipless basket. The largest calculus removed with the basket was an 8 x 3mm calculus which was in alignment with the duct. The majority of the calculi removed by basket were not more than 4-5mm. All calculi removed through the basket were fully visible through sialendoscopy and freely mobile. Larger and adherent stones were removed with the help of a combined approach sialendoscopy, transfacial approach in the case of parotid calculi and the transoral approach in submandibular calculus.9,10 It was observed that partially hidden calculus was difficult to extract with the help of a basket alone. In some cases, the ductal angulation was unfavourably aligned and hence an end-on view of the calculus was not available. We did not have any displaced calculus in this series. Intraglandular calculus was invariably hidden partially in the second or third-level duct system which was difficult to remove. Some micro calculi were removed with the help of lavage. In one case, a small stone of 2 mm was removed with distal sialodochotomy due to distal papillary stenosis. Sialendoscopy missed calculus during the first attempt due to mucosal oedema. There was one case where a parotid calculus was not visible with sialendoscopy and was detected using intraoperative ultrasound and same removed using a transfacial combined approach. Intraoral submandibular calculi in the proximal third of the duct and intraglandular location are difficult to remove due to poor accessibility and need expertise. Bulky tongue, retroclined teeth and short neck added to the difficulty. Such stones may be removed with the help of robotic-assisted sialolithotomy with sialendoscopy (RASS).12 Almost all patients of sialolithiasis had symptomatic improvement with a single procedure and there was no recurrence of symptoms noted after one year. The stone size and shape showed no significant effect on the outcome. In our study, no sialadenectomy was performed. But there are studies in which sialadenectomy was done in view of the difficulty in the retrieval of calculus.7
In the immediate post-op period, some patients had numbness in the tongue after submandibular sialendoscopy with a transoral approach in the immediate post-operative period but that improved in all the patients after the 1-month post-op period. Difficulties encountered during the procedure included retroclined teeth, trismus, short neck and cervical spine issues, failure to identify and dilate the papillae, masseteric bend which was non-negotiable, not being able to visualize the hilar area or beyond, slipped calculus and large calculus. In the case of large calculus, sialendoscope was used to locate the stone and was removed by a combined approach -transfacial in the case of parotid sialendoscopy and transoral in the case of submandibular sialendoscopy.7,11 All our patients underwent the procedure under general anaesthesia mainly under nasal intubation. Deviated nasal septum and adenoids sometimes posed problems with nasal intubation resulting in nasal bleeding which settled with packing. In one patient there was an inadvertent middle turbinate injury after the procedure. There are centres where sialendoscopy was done as a day-care procedure under local anaesthesia. While doing repeated procedures and after all parotid sialendoscopies (since the parotid duct is more prone to stricture formation) stenting was done. We had noticed extrusion of the stent as a complication for whom revision procedures were needed for early extrusion. In the study population, no patients underwent sialadenectomy. However, there are studies in which sialedenectomy was performed in failed cases.7
In the 65 patients with sialolithiasis, the mean COSS scores decreased after sialendoscopy and the improvement persisted at 1 year of follow-up. In the case of sialolithiasis, the success rate was 100%. Almost all patients of sialolithiasis had good outcomes postoperatively and persisted after 1 year which was similar to the study conducted by Evren Erkull et al.2, 4,13 The outcome assessed in this study were the cases done during the last two years and not from the period of the first sialendoscopic procedure done in this institute. A learning curve in interventional Sialendoscopy requires at least 30 cases to reach satisfactory operation time and performance rating. Both parameters showed continuous improvement after 50 cases.12
Even though sialendoscopy has a gradual and slow learning curve, once mastered it provided good long-term outcomes with fewer complications. Results after sialendoscopy were stable upto the first postoperative year of follow up for sialolithiasis
CONCLUSION
Interventional sialendoscopy showed good outcomes which persisted after 1 year in the case of sialolithiasis. Sialendoscopy for intraductal sialolithiasis did not require a repeat procedure in the majority of the cases irrespective of the size and site of the calculus. Sialolithiasis of both parotid and submandibular glands showed good outcomes. The use of a combined approach technique and intraoperative radiology improved calculus retrieval in sialolithiasis. Sialendoscopy as a minimally invasive procedure has good outcomes in obstructive inflammatory conditions of salivary glands.
STRENGTH AND LIMITATIONS
Only a subjective assessment was done for the patient. More studies with an objective assessment like measurement of salivary flow rate and technechium scintigraphy can be done.
Questionnaires like Multidisciplinary salivary gland society questionnaire(MSGS) can be utilised specifically for salivary glands to assess the complications of sialendoscopy.
End Note
Author Information
- Dr Bini Faizal
Professor, Department of ENT, Amrita Institute of Medical Sciences, Amrita Vishwa Vidyapeedham University, Kochi, India.
Email- binifaizal@gmail.com Phone: +91- 9446990937 - Dr Ammu Dileep
Junior Resident, Amrita Institute of Medical Sciences, Kochi, India.
Phone: +91 9809740181
Email- ammusdileep1993@gmail.com - Greeshma CR
Lecturer, Department of Biostatistics, Amrita institute of Medical Sciences, India.
Phone:+919544427706
Email: greeshma134@gmail.com
Acknowledgements: Department of radiology, Amrita Institute of medical sciences, Kochi
Funding Source: There was no funding from any external agency.
Conflict of Interest: None to declare.
Ethical Standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation (please name) and with the Helsinki Declaration of 1975, as revised in 2008.
Author Contributions:
Dr Bini Faizal: Contributed to the conception, design and analysis of data; revised critically for intellectual content, final approval and is accountable for the accuracy of the work
Dr Ammu Dileep: Contributed to acquisition of data, analysis and interpretation; drafting of article.
Mrs Greeshma C R: Contributed to the methodology, analysis and interpretation of data; drafting and interpretation of results
REFERENCES
- Capaccio P, Torretta S, Ottaviani F, Sambataro G, Pignataro L. Modern management of obstructive salivary diseases. Acta Otorhinolaryngol Ital. 2007 Aug;27(4):161–72.
[Pubmed] - Callander JK, Plonowska-Hirschfeld K, Gulati A, Chang JL, Ryan WR. Symptom Outcomes After Sialendoscopy-Assisted Salivary Duct Surgery: A Prospective 6-Year Study. Laryngoscope. 2023 Apr;133(4):792–800.
[Pubmed] | [Crossref] - Aubin-Pouliot A, Delagnes EA, Eisele DW, Chang JL, Ryan WR. The Chronic Obstructive Sialadenitis Symptoms Questionnaire to assess sialendoscopy-assisted surgery. Laryngoscope. 2016 Jan;126(1):93–9.
[Pubmed] | [Crossref] - Aubin-Pouliot A, Delagnes EA, Chang JL, Ryan WR. Sialendoscopy-assisted surgery and the chronic obstructive sialadenitis symptoms questionnaire: A prospective study. Laryngoscope. 2016 Jun;126(6):1343–8.
[Pubmed] | [Crossref] - Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990 Jun;19(3):135–8.
[Pubmed] | [Crossref] - Zenk J, Koch M, Klintworth N, König B, Konz K, Gillespie MB, et al. Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg. 2012 Nov;147(5):858–63.
[Pubmed] | [Crossref] - Moorthy A, Bachalli PS, Krishna S, Murthy S. Sialendoscopic Management of Obstructive Salivary Gland Pathology: A Retrospective Analysis of 236 Cases. J Oral Maxillofac Surg. 2021 Jul;79(7):1474–81.
[Pubmed] | [Crossref] - Walvekar RR, Carrau RL, Schaitkin B. Endoscopic sialolith removal: orientation and shape as predictors of success. Am J Otolaryngol. 2009;30(3):153–6.
[Pubmed] | [Crossref] - Koch M, Zenk J, Iro H. Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin North Am. 2009 Dec;42(6):1173–92, Table of Contents.
[Pubmed] | [Crossref] - Fritsch MH. Algorithms for treatment of salivary gland obstructions without access to extracorporeal lithotripsy. Otolaryngol Clin North Am. 2009 Dec;42(6):1193–7.
[Pubmed] | [Crossref] - Razavi C, Pascheles C, Samara G, Marzouk M. Robot-assisted sialolithotomy with sialendoscopy for the management of large submandibular gland stones. Laryngoscope. 2016 Feb;126(2):345–51.
[Pubmed] | [Crossref] - Schwartz N, Hazkani I, Goshen S. Combined approach sialendoscopy for management of submandibular gland sialolithiasis. Am J Otolaryngol. 2015;36(5):632–5.
[Pubmed] | [Crossref] - Erkul E, Çekin E, Güngör A. Long-Term Outcomes of Sialendoscopy in the Management of Sialolithiasis and Idiopathic Chronic Sialadenitis with Ductal Scars. Turk Arch Otorhinolaryngol. 2019 Jun;57(2):75–80.
[Pubmed] | [Crossref]