Perspective Published on December 30, 2022
Competency Based Medical Education (CBME) – The ENT Perspective
Suchit Roy B R1
1. Department of ENT, Government Medical College, Thiruvananthapuram*
Competency Based Medical Education (CBME) - What is it?
It was in 1997 that Graduate Medical Education Regulations were last introduced by the Medical Council of India. With more than a decade and a half elapsing since those regulations came into force, there was a need for a relook. With the aim of creating a medical graduate competent to serve the community after successful completion of the undergraduate medical course, the Medical Council of India revamped the medical education system in India to one of Competency Based Medical Education. After about four years of work on it by committed medical teachers from across the country, the curriculum was implemented from the 2019 batch of students.1 This brought about a paradigm shift in Medical Education in the country.
CBME has been defined as an outcome-based approach of medical education using a framework of competencies. Competency is an observable activity of the health professional with a judicious and consistent mix of knowledge, skills, attitudes, and communication. Competency is not an all or none phenomenon; it is incremental. It is not about demonstration of discrete skills by the learner but the integration and application of knowledge, skills, attitudes, and communication in the context of a patient rather than any one of these in isolation. Competency is individual and context specific. Competencies are acquired in different time frames by different learners. The same is true for different competencies for the same learner. This mandates the need for an ongoing and longitudinal assessment of the learner and decides whether they need further or different learning opportunities to acquire competency. Hence, there is a need for consistent and continuous assessment of the learner. The assessment has again been made competency based.
The aim here is to evaluate CBME, specifically from an ENT perspective. In CBME, there are 120 ENT competencies to be acquired by a learner over two phases. Of these, 76 are purely ENT and 44 are integrated with other specialties viz – 17 with Anatomy, 4 with Physiology, 1 with Community Medicine, 4 with Dermatology, 1 with Internal medicine, 16 with Pediatrics and 1 with General Surgery. Therefore, assessment in competency-based curriculum should incorporate integration to the extent feasible while maintaining subject identity.
Teaching learning methods (TLMs) too have undergone a sea of change. Didactic lectures have taken a back seat. Other TLMs like Small Group Discussions SGDs), seminars, Bed-side Teaching, DOAP (Demonstrate Observe Assist Perform), Learner Doctor Method or Clinical Clerkship (learner follows up a patient in the ward from admission to discharge), Self-directed learning (SDL) are a few which have been suggested as TLMs.
The Competencies2
Each subject competency is numbered. The initial two alphabets denote the subject. This is followed by numbers. The first number denotes a major header and the second number followed by a period is a sub header.
EN1 is anatomy, physiology, and pathophysiology (EN2.1 to EN2.15) EN2 is clinical skills EN2.1 to EN2.15). EN3 is diagnostic and therapeutic skills (EN3.1 to EN3.6) and EN4 is management of ENT disorders (EN4.1 to EN4.53)
- EN1.1 Describe the Anatomy & physiology of ear, nose, throat, head & neck
Domain: Knowledge
Level: Knows how
TLM: Lecture / SGD
Assessment: Written / VIVA
- EN2.2 Demonstrate the correct use of a headlamp in the examination of the ear, nose, and throat
D: Skill
L: Shows how
TLM: DOAP session
Assessment: Skill assessment / OSCE
- EN2.3 Demonstrate the correct technique of examination of the ear including Otoscopy
D: Knowledge / Skill / Attitude
L: Shows how
TLM: DOAP session / Bedside clinic
Assessment: Skill assessment / OSCE
- EN2.1 Elicit document and present an appropriate history in a patient presenting with an ear discharge
D: Knowledge / Skill / Attitude / Communication
L: Shows how
TLM: Lecture / SGD / Demonstration
Assessment: Skill assessment / OSCE
Integrated topics are as follows
- Anatomy (AN): Tonsil, soft palate, hypopharynx, Waldeyer’s ring, nose, PNS, larynx, RLN, hypoglossal nerve, external, middle, and inner ears
- Physiology (PY): Smell and taste, hearing physiologies, auditory pathway, hearing tests, testing hearing taste & smell in volunteers
- Community Medicine (CM): Health hazards of air, water, noise, radiation pollution
- Dental (DE): Cancer oral cavity, precancerous lesions and their identification, Counsel patients on risks of oral cancer with respect to tobacco, smoking, alcohol, and other causative factors
- Internal Medicine (IM): Hearing loss in the elderly etiology, clinical features, management, rehabilitation
- Pediatrics (PE): Kerosene ingestion, nasopharyngitis, pharyngotonsillitis, AOM, epiglottitis, Acute LTB, stridor in children including history taking, FB aspiration in infants and children, examination of ear (otoscope), nose, throat, X-rays of PNS, mastoid and chest in FB aspiration, allergic rhinitis ad atopic dermatitis in children
- General Surgery (SU): Etiopathogenesis of oral cancer, symptoms, and signs of pharyngeal cancer - appropriate investigations and principles of treatment.
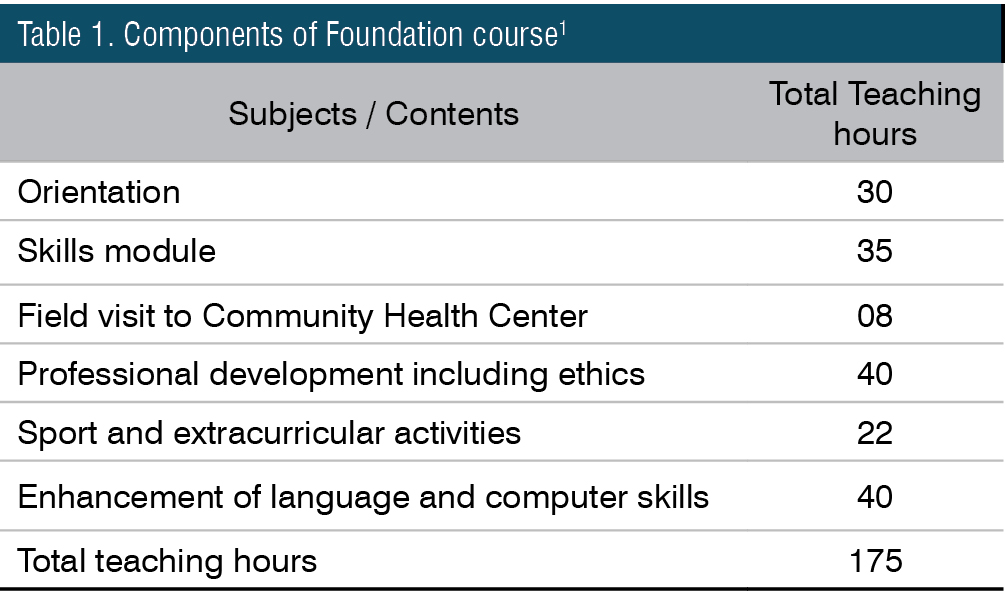
The course1
The total duration of study is 54 months followed by 12 months of internship. Medical Education now starts with a foundation course of one month duration. The aim is to sensitize the fresh medical student with the required knowledge and skills that will assist him/her in acclimatizing to the new professional environment which would be his/her milieu for a life-long career in the medical profession. The components of foundation course are as in the table below (Table 1).
The whole course is divided into three phases, with the third phase again divided into two parts. Phase I is 13 months duration including examinations, with study of Anatomy, Biochemistry, Physiology, AETCOM, and Community Medicine, culminating with exams in Anatomy, Biochemistry, Physiology. Sensitization of Phase I students are done by Early Clinical Exposure3 (ECE). Students are taken in batches to clinics for ninety hours during this Phase. AETCOM4 (Attitudes, Ethics and Communication) is an integral part of CBME and is part of all phases of study. Phase II starts immediately after Phase I, even before the results are out.
Those who fail in Phase I, go back, and attempt the failed subjects in a month’s time, but never later than three months and can save a year (SAY). Those who pass this supplementary exam can join their original batch and continue their studies. The clinical classes lost during their exams are to be compensated by extra classes. Those who fail, join the succeeding batch. There are no supplementary batches in the CBME framework. Only four attempts are permitted per subject, including the SAY exams, failing which they must quit the course.
Phase II duration is 12 months including examinations. Learners undergo training in Microbiology, Pathology, Pharmacology, AETCOM, Postings are in Internal Medicine, General Surgery, Obstetrics and Gynecology, Pediatrics, Orthopedics, Community Medicine, Forensic Medicine, Otorhinolaryngology (4 weeks), Ophthalmology, Psychiatry, Respiratory Medicine, Radiodiagnosis, Dermatology and Dental. The phase ends with examinations in Microbiology, Pathology and Pharmacology. Clinical posting in Otorhinolaryngology is four weeks duration, three hours a day, five days a week.
Phase III Part I is of 13 months (including exams) with study of Community Medicine, Forensic Medicine, Otorhinolaryngology (4 weeks), Ophthalmology, AETCOM, Internal Medicine, General Surgery, Obstetrics and Gynecology, Pediatrics, Orthopedics, Psychiatry, Respiratory Medicine, Radiodiagnosis & Radiotherapy, Dermatology, Anesthesia and Casualty. Clinical posting in Otorhinolaryngology is four weeks duration, three hours a day, six days a week. End of phase assessment would be for Community Medicine, Forensic Medicine, Ophthalmology and Otorhinolaryngology.
Phase III Part I is followed by two months of electives.5 This is to provide the learner with opportunities for diverse learning experience and to do research / community projects that will stimulate enquiry, self-directed, experiential learning, and lateral thinking. This is designed to be in two blocks of four weeks each. Block I would be in preclinical or para-clinical or basic sciences laboratory or under a researcher in an ongoing research project. Block II would be in a clinical department including specialties, super-specialties, ICUs, blood bank and casualty.
Finally comes Phase II Part II. Duration of postings is 13 months including one month of exams. Clinical postings are in Internal Medicine, General Surgery, Obstetrics & Gynecology, Pediatrics, Orthopedics and AETCOM. Summative assessment would be for Internal Medicine, General Surgery, Obstetrics & Gynecology, Pediatrics and Orthopedics.
Logbooks1 have been made mandatory for all subjects, where competency acquisitions are certified. They also have reflections of students on their learning. Portfolios are where they record how they acquired competency viz. clinical case recordings, OP notes, operative procedures, pictures etc. Logbook certification is an eligibility criterion for applying for University examinations. It is mandated that they certify even the non-exam subjects, to be eligible to apply for end of phase University examinations. Logbooks would come to a minimum of 24 in number, including one for AETCOM.
Assessment6
The assessment is as follows.
- Phase II / Phase III Part I
- End of posting exam
- Internal assessment (theory)
- Final Internal Assessment
- Clinical exam
- Internal assessment (theory)
- University exam
- Theory 100 marks
- Clinical + VIVA 100 marks
Internship7
This would be for a minimum period of twelve months. CRRI (Compulsory Rotatory Residential Internship) has been renamed CRMI (Compulsory Rotatory Medical Internship) The residential tag has been removed.
The Pros
- Good concept if implemented earnestly
The CBME concept is exceedingly good. Stress is on acquisition of competencies and testing these rather than rote memorization and the knowledge domain only. If implemented in earnest, This shall produce primary care physicians adept with all basic competencies to serve the community.
- Certification, which was lax previously, has been made mandatory
Every learning activity of the student is recorded. Logbooks have not only been made compulsory, but certification made mandatory for eligibility to appear for the University examinations also. Up to twenty percent IA marks (Theory and Practical) should be from logbook assessment.
- Attendance and marks compulsory and limits raised
80% attendance in theory and clinics separately is mandatory to be eligible to appear for the University examinations. Separate 80% attendance is required for each phase of postings.
Students must secure at least 50% marks of the total marks (combined in theory and practical / clinical; not less than 40 % marks in theory and practical separately) assigned for internal assessment in a particular subject to be eligible for appearing at the final University examination of that subject.
There shall be no less than two examinations in each clinical subject in a professional year. A student who has not taken the minimum required number of tests for IA each in theory and practical will not be eligible for university examinations. When subjects are taught in more than one phase, the internal assessment must be done in each phase and must contribute proportionately to final assessment. Internal assessment marks will not be added to University examination marks and will reflect as a separate head of passing at the summative examination.
- Vertical and horizontal integration made mandatory8
Integration, both horizontal (inside the phase) and vertical (between phases) starts from Phase I. This helps to create awareness among students of the importance of basic sciences in clinical sciences. Wherever possible, NMC insists on alignment (teaching same topics across specialties simultaneously – when dissection of thyroid takes place in anatomy, thyroid physiology and thyroid function tests are taught in physiology and biochemistry respectively) of topics too.
- New topics of relevance added
New topics like health hazards of air, water, noise and radiation pollution, national programs, informed consent, counselling have been added in tune with changes happening in society. The relevance of these topics is high but were neglected in the previous curriculum.
Others like anatomy of head, pathophysiology of ENT diseases, smell and taste disorders, topical medications in ENT, microbiological and histopathological investigations have also been added and are welcome changes.
- AETCOM
This is a new addition to the curriculum and a very important one too. In this era of conflict between doctors and the society, AETCOM is the need of the hour. AETCOM is integral part of all phases. A short answer question on AETCOM is mandatory in theory assessment and desirable that this is assessed in clinical examinations as well.
Separate logbook of AETCOM for all phases together has also been introduced by the KUHS. 80% attendance in AETCOM is mandatory to be eligible to appear for examinations.
- Extracurricular activities1
These have been integrated into the curriculum and separate hours earmarked in the curriculum itself. This should promote all-round development of the student.
The Cons
- Tough on students and teachers
The sudden change in the curriculum has put students and teachers in a tangle. Clinical postings have been cut short to three hours per day from the previous four/five hours. Medical colleges with 250 students find it difficult to demonstrate and check acquisition of competencies by learners. About 50 students are to be attended to in three hours. Students opine that they find it difficult to prepare for seminars and maintain logbooks. Many teachers are yet to be trained in CBME and are not used to the curriculum. Different institutions follow different training schedules.
- Infrastructure deficits
Lack of infrastructure is a bottle neck in teaching. SGDs are to be conducted with about 15 students in a batch. Large medical colleges require at least three classrooms simultaneously to cater to students of a single batch. Lack of adequate number of classrooms result in clubbing of batches and the purpose of SGD is defeated. The semester system in the previous curriculum has been done away with, resulting in two or three batches of different years coming for posting simultaneously. Major departments like Internal Medicine, General Surgery, OBG can have Phase II, Phase III Part I and Phase III Part II students of different years coming for postings simultaneously. ENT, Ophthalmology, and other specialties can have Phase II and Phase III Part I students of different years coming for postings together. This requires additional space and classrooms, which many institutions lack at present.
- Manpower deficits
Lack of an adequate number of faculty hampers teaching. NMC mandates that the minimum faculty required in ENT for 100 admissions are one Professor, Associate Professor, Assistant Professor and Senior resident each. For 250 admissions these are one Professor and Associate Professor each and two each of Assistant Professors and Senior residents. It is practically impossible to conduct OPD, ward work, OT work and engage several batches of students simultaneously. If one or two of the faculty go on leave / duty off, of which they are rightfully privileged, things go awfully wrong. Two internal exams per phase is what NMC envisages, but it is heavy load conducting and evaluating for large batches of students. The NMC stipulates two internal examiners and two external examiners from outside the university / state for the conduct of final summative examinations. With the NMC prescribing a pan-India timetable for the undergraduate course, and examinations happening almost simultaneously all over India, it would be practically impossible to get two out of state / university examiners for the conduct of examinations.
- Questionable omissions and additions of topics
Topics of importance like complications of otitis media, hearing defects in infants and children, hearing aids and cochlear implantation, diseases of external nose, CP angle diseases, voice and speech disorders, endoscopies, LASER, and other newer technologies are completely omitted. Kerosene ingestion has been added as part of integration with Pediatrics (PE14.2)
Conclusion
CBME has been introduced and it is here to stay. The earlier we adapt to it, the better for students as well as teachers. There definitely are some technical difficulties during implementation; expectedly for programs of this magnitude introduced all over the country. The Heads of Departments of ENT of all medical colleges had met several times online and a consensus was arrived at on logbook and mark divisions for theory and practical examinations. More such meetings, frequent interaction between stakeholders and teachers and more teacher training programs would go a long way in alleviating at least some of these problems to a great extent.
End Note
Author Information
- Dr. Suchit Roy B. R., Professor, Department of ENT, Government Medical College, Thiruvananthapuram;
Member Board of studies (UG), KUHS
Conflict of Interest: None declared
References
1. Regulations on Graduate Medical Education (Amendment), 2019, by The Gazette of India (Extraordinary), New Delhi, Wednesday, November 6, 2019 / Kartika 15, 1941
2. Medical Council of India, Competency based Undergraduate curriculum for the Indian Medical Graduate, 2018. Vol. 3
3. Medical Council of India. Early Clinical Exposure for the Undergraduate Medical Education Training Program, 2019
[Source]
4. Medical Council of India. Attitude, Ethics and Communication (AETCOM) Competencies for the Indian Medical Graduate, 2018
[Source]
5. Medical Council of India. Electives for the Undergraduate Medical Education Training Program, 2020
[Source]
6. Medical Council of India. Competency Based Assessment Module for Undergraduate Medical Education Training program, 2019
[Source]
7. The National Medical Commission (Compulsory Rotating Medical Internship) Regulations, 2021, by the Gazette of India (Extraordinary), New Delhi, Thursday, November 18, 2021 / Kartika 27, 1943
8. Medical Council of India. Alignment and Integration Module for Undergraduate Medical Education Program, 2019
[Source]