Case Report Published on December 30, 2022
Blunt Cerebrovascular Injury with Delayed Ischemic Stroke - A Case Report with Discussion on Diagnosis and Management
Vidya Aravind1, Jayalekshmi A1, Shaira K P1
ABSTRACT
Blunt cerebrovascular injury(BCVI) can cause devastating morbidity and mortality. The problem with BCVI is that most physicians and health workers are not aware of this condition. It can present with periods of a varying time frame of about 12 to 36 hours or as late as 1 week after trauma. This may result in the complacent attitude of health workers that all is well given the initial normal finding in CT. This article aims at highlighting the importance of early diagnosis and treatment, to prevent and halt the progression of the injury into stroke and its resultant morbid consequences. This case report is that of a young male patient who came to the casualty with a history of assault and neck injury. He was hemodynamically stable and was managed with suturing of the wound. Initial imaging did not reveal any vessel injury, but he developed a stroke 36 hours later. A brief commentary on causes, presentation, early diagnosis, and management is described.
Introduction
Symptoms similar to BCVI were initially described in 1945 by Ecker in 3 cases of neck injury by missile.1 It is a rare occurrence, but can cause severe morbidity and even mortality and hence needs to be addressed as an emergency. Often missed because initial CT imaging may not reveal any findings. The examining doctors are falsely reassured as the patient is hemodynamically stable with no neurological signs in the early period after trauma. With an increase in road traffic accidents, the incidence of BCVI is also increasing. So it is pertinent that the medical fraternity is aware of this condition in post-trauma patients. Vertebral, Carotid artery, and sometimes veins are involved. In many cases, the diagnosis may be missed because of associated severe head and chest injuries. Apart from RTA and assault, other causes are contact sports, snowboarding, skiing, fall from height, bungee jumping, and strangulation.2 Early diagnosis and thrombolytic therapy can prevent progression into an ischemic stroke. This is a case report of a young active male who developed BCVI after an assault. The case was admitted to the ENT ward as USG and CT imaging did not show any evidence of intracranial bleeding. The patient developed global aphasia about 24 hours later which was mistaken for functional aphonia due to Post-traumatic stress disorder. 12 hours later he developed hemiparesis. The delayed presentation may be due to minimal intimal injury which was missed in the initial scan. This case report discusses the clinical presentation, the findings which should be diligently checked in imaging, the need for meticulous follow-up, detecting even subtle variations in neurological signs, and ensuring early prophylactic and therapeutic intervention.
Case report
A 28-year-old male who works as a refractionist was brought to the casualty at night with a history of assault with a broken bottle. He was conscious and well-oriented, and his vitals-pulse, BP, RR, and SpO2 were normal. He had a 6cm X 1cm lacerated would just below the left angle of the mandible with minimal bleeding. He had no evidence of a foreign body, injury to deep structures, or laryngeal airway. This was corroborated by USG and CT imaging. However, his voice was hoarse. Video laryngoscopy showed left vocal cord paresis with congestion over the left aryepiglottic fold and falling forward of the left arytenoid. He was started on injection of Ceftriaxone and injection Dexona because of left vocal cord palsy. 24 hours later he was reported to be irritable. A surgery consultation and repeat CT scan were done which revealed no intracranial bleed or ischemia. This event coincided with his wife’s visit to see him. This was followed by global aphasia, which was wrongly attributed to post-traumatic stress disorder and functional aphonia. A psychiatry consultation was also done. All this while the patient had normal BP and was conscious. The next morning after about 36 hours he was found to have right-sided hemiparesis with grade 3 power in both upper and lower limbs. Suspecting dissection, Doppler was done but showed normal flow in neck vessels. This time the CT imaging showed left middle cerebral artery stem occlusion with infarct. Neurology consultation was done and anti-platelet therapy was started. The patient is on drugs, physiotherapy, and speech therapy.
BCVI-Blunt Cerebrovascular Injury-Discussion
to begin with, most BCVI cases are asymptomatic. Awareness of this condition is low as incidence is only 1 to 2.7%.3 Causes are mainly due to high-velocity trauma as in RTA. It can occur in falls from height, strangulation, contact sports injuries, and trauma to the oropharynx with a penetrating object.4,5 Very rarely it can occur in low-velocity injuries as in maneuvers by a chiro practitioner, and yoga posture. It has also been reported in nose blowing, and vomiting, although the exact mechanism has not been explained. Connective tissue disorder and Ehlers-Danlos syndrome can cause spontaneous BCVI.6 It can be associated with cervical spine injuries. Neck vessels can undergo twisting, stretching, compression, and even transection.7 Vessels can be caught between the vertebra and mandible, occipital condyle, and atlas. In the event of transection, the findings are immediate and the patient is in shock. At the time of presentation, the patient is hemodynamically stable with no neurological signs. The imaging may also be uneventful. With a varying period of latencies of 18 to 24 hours or as late as 1 week, the patient can present with ischemic stroke. This is due to a thrombus being formed at the site of the intimal tear with progressive occlusion or embolic episodes.8 Few patients can present with pulsatile tinnitus, amaurosis fugax, or Horner’s syndrome.9 Stroke should be managed with stroke protocol like thrombolytics, thrombectomy, and endovascular intervention. The problem with BCVI is the failure to diagnose this early on. Plain CT imaging cannot pick up early infarcts and a normal scan can induce a complacent attitude by the treating personnel. This can fail to detect subtle signs of stroke, like irritability and global aphasia. In our case, the failure to respond to queries was taken to be functional aphonia attributed to Post-traumatic stress disorder. This resulted in a delayed diagnosis. The mechanism of injury is intimal tear dissecting through the layers resulting in thromboembolism. Vasavasorum bleeding can lead to intramural hematoma and progressive vessel wall narrowing Aneurysm from focal outpouching can lead to narrowing of the vessel and in rare cases even rupture.
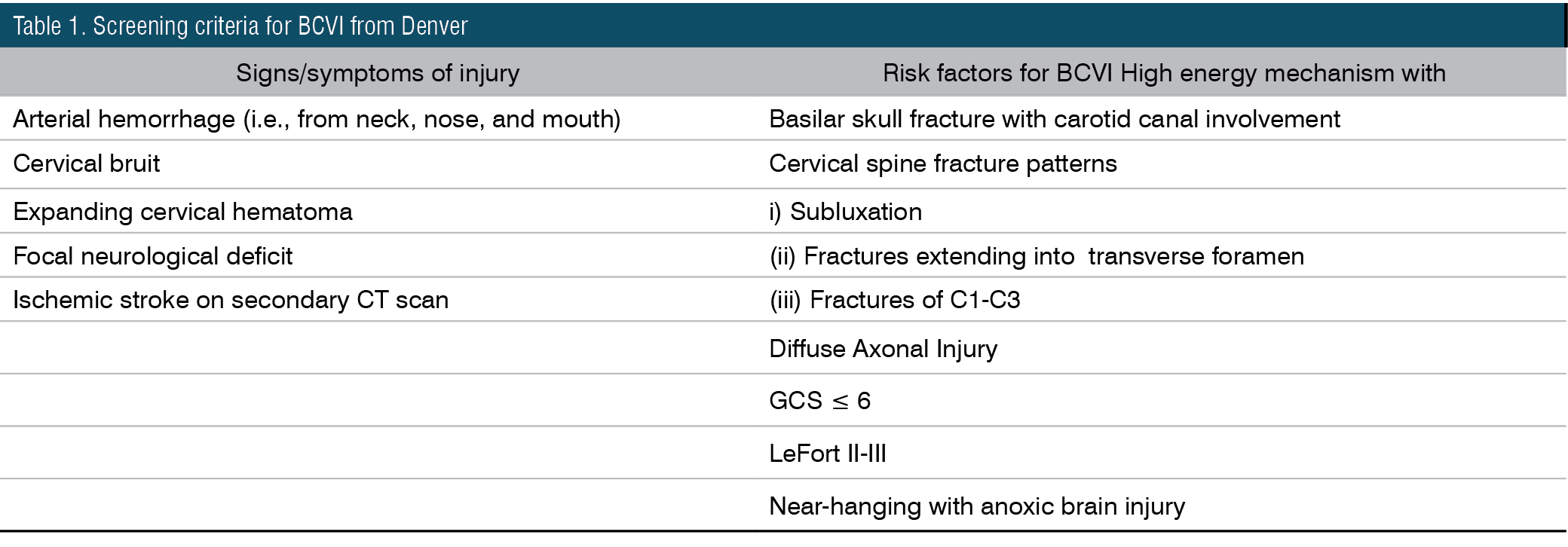
It’s important to know when to do imaging. One should look for focal neurological signs or signs that do not correlate with CT findings.9 Clinically if there is hemodynamic instability and evidence of expanding hematoma, imaging should be done.4 Vessel angiography was the gold standard investigation for dissection and BCVI. Nowadays CT angiography, MRA, and Duplex ultrasonography are the alternative investigations. Findings to be noted are the integrity of the intima, intramural hematoma, aneurysm, narrowing, stenosis, and transection. It would be helpful to note the grading of severity. Doppler can detect flow anomalies and thrombi. Denver criteria (Table 1) is a screening tool for BCVI based on mechanism, pattern, and symptoms of injury.10 This has a sensitivity of 97% and a specificity of 42%. Other criteria that are followed are Western Trauma Association, EAST-Eastern Association for the Surgery of Trauma, and Memphis criteria (Table 2).

For the feasibility of the approach, the neck is divided into 3 zones. Zone 1 is above the hyoid, Zone 3 is below the cricoid, and zone 2 is in between 1 and 2. Zone 2 can be approached by an open surgical approach, whereas zone 1 and 2 are difficult to be addressed surgically and hence may require an endovascular approach.
In grade I (Biffl’s classification) initial thrombolytic therapy may suffice.11,12 It is followed by anti-platelet therapy until the intimal tear is healed. This may take up to 2 to 3 months and may recover completely. Grade I and II are mild and on treatment grade II may improve to grade I level (Table 3). If there is worsening or progression to grade III, then medical treatment may not suffice. Endovascular intervention or an open surgical approach may be needed. Grade IV, that is arterial obstruction is mitigated by the stent and lifelong anti-platelet therapy. Arterial transection, Grade V is managed by repair and grafting.14,15 Surgical or endovascular intervention is also done if the patient is hemodynamically unstable if signs of expanding hematoma apart from the above radiological worsening of grading. Follow-up CT angiography is done 7 to 10 days later.

If ENT or neck bleed or injury occurs, prophylactic anticoagulant therapy with Heparin may be started irrespective of CT imaging as false negative results are common.10 U/kg/hr of Heparin infusion is given maintaining a target PTT of 40 - 50 seconds to reduce hemorrhagic complications. Clopidogrel or Aspirin is used as antiplatelet therapy in those patients not tolerating anti-coagulants.16
Conclusions
With the increase in high-velocity RTA, incidences of BCVI should be kept in mind as stretching of neck vessels can occur This patient presented with assault and hoarseness due to left recurrent laryngeal palsy. Even though the patient did not have any hemodynamic instability, the possibility of subtle intimal injury should be kept in mind in every neck trauma case. Cursory imaging of neck vessel integrity should be done away with and the patient should be followed up with a repeat USG or CT angiography. Awareness of global aphasia should be emphasized among the trauma personnel and should not be brushed away as functional aphonia due to post-traumatic stress disorder.3 Prophylaxis with antithrombotic agents may be started in neck injury cases. Patient symptoms should be graded according to severity and progression checked frequently. If the grading becomes severe, the management may have to be changed accordingly, ranging from an open surgical approach in vessel transection with grafting, to an endovascular approach with stenting or coiling in case of an aneurysm. Cases may require prolonged prophylactic antiplatelet therapy. They have to be followed lifelong. It is important to emphasize screening for BCVI in trauma cases as progression to stroke is associated with morbidity and mortality.
End Note
Author Information
- Dr. Vidya Aravind, Junior Resident, Department of ENT, Government T D Medical College, Alappuzha
- Dr. Jayalekshmi A, Junior Resident, Department of ENT, Government T D Medical College, Alappuzha
- Dr. Shaira K P, Associate Professor, Department of ENT, Government T D Medical College, Alappuzha
Conflict of Interest: None declared
References
1. Ecker A, Riemenschneider PA. Arteriographic evidence of spasm in cerebral vascular disorders. Neurology. 1953 Jul;3(7):495–502.
[Pubmed] | [Crossref]
2. Walsh BA, Gregorie WD, Whittle JS. Deconstructing Dissections: A Case Report and Review of Blunt Cerebrovascular Injury of the Neck. Case Rep Emerg Med. 2018 Aug 8;2018:6120781.
[Pubmed]| [Crossref]
3. Karamchandani R, Rajajee V, Pandey A. The role of neuroimaging in the latent period of blunt traumatic cerebrovascular injury. Open Neuroimag J. 2011;5:225–31.
[Pubmed] | [Crossref]
4. Hon K, Roach D, Dawson J. A case report of blunt intraoral cerebrovascular injury in a child following intraoral trauma: The pen is mightier than the sword. Trauma Case Rep. 2021 Dec 8;37:100567.
[Pubmed] | [Crossref]
5. Cuellar TA, Lottenberg L, Moore FA. Blunt cerebrovascular injury in rugby and other contact sports: case report and review of the literature. World J Emerg Surg. 2014;9:36.
[Pubmed] | [Crossref]
6. Sharma P, Hegde R, Kulkarni A, Sharma S, Soin P, Kochar PS, et al. Traumatic vertebral artery injury: a review of the screening criteria, imaging spectrum, mimics, and pitfalls. Pol J Radiol. 2019 Aug 20;84:e307–18.
[Pubmed] | [Crossref]
7. Al-Harthy A, Al-Hinai A, Al-Wahaibi K, Al-Qadhi H. Blunt Cerebrovascular Injuries A review of the literature. Sultan Qaboos Univ Med J. 2011 Nov 1;11(4):448–54.
[Source]
8. Anyama B, Treitl D, Wessell J, Solomon R, Rosenthal AA. Delayed Stroke following Blunt Neck Trauma: A Case Illustration with Recommendations for Diagnosis and Treatment. Case Rep Emerg Med. 2017;2017:3931985.
[Pubmed] | [Crossref]
9. Blunt Cerebrovascular Injury - Practice Management Guideline [Internet]. [cited 2023 Mar 15].
[Source]
10. Kobayashi K, Imagama S, Okura T, Yoshihara H, Ito Z, Ando K, et al. Fatal case of cervical blunt vascular injury with cervical vertebral fracture: a case report. Nagoya J Med Sci. 2015 Aug;77(3):507–14.
[Pubmed]
11. Beliaev AM, Civil I. Multidetector CT angiography influences the choice of treatment for blunt carotid artery injury. BMJ Case Rep. 2014 Aug 6;2014:bcr2013200659.
[Pubmed] | [Crossref]
12. Frink M, Haasper C, Ringe KI, Krettek C, Hildebrand F. Blunt cerebrovascular trauma causing vertebral arteryd issection in combination with a laryngeal fracture: a case report. J Med Case Reports. 2011 Aug 15;5:381.
[Pubmed] | [Crossref]
13. Weber CD, Kobbe P, Herren C, Mahnken AH, Hildebrand F, Pape HC. Endovascular Management of a Combined Subclavian and Vertebral Artery Injury in an Unstable Polytrauma Patient: Case Report and Literature Review. Bull Emerg Trauma. 2017 Jan;5(1):53–7.
[Pubmed]
14. Ariyada K, Shibahashi K, Hoda H, Watanabe S, Nishida M, Hanakawa K, et al. Bilateral Internal Carotid and Left Vertebral Artery Dissection after Blunt Trauma: A Case Report and Literature Review. Neurol Med Chir (Tokyo). 2019 Apr 15;59(4):154–61.
[Pubmed] | [Crossref]
15. Nguyen HS, Oni-Orisan A, Cochran J, Pollock G. Resection of a recurrent cervical internal carotid artery pseudoaneurysm after failed endovascular therapy. Surg Neurol Int. 2016 Jan 7;7(Suppl 2):S49–52.
[Pubmed] | [Crossref]
16. Murphy PB, Severance S, Holler E, Menard L, Savage S, Zarzaur BL. Treatment of asymptomatic blunt cerebrovascular injury (BCVI): a systematic review. Trauma Surg Acute Care Open. 2021;6(1):e000668.
[Pubmed] | [Crossref]